Text
INTRODUCTION
The relationship between patients and doctors has always been asymmetrical since its inception. In the 19th century, scientific discovery helped physicians practice medicine with a better understanding of afflictions and diseases based on anatomy. It signified an irreversible departure from witchcraft and humoral therapy.
Becoming a doctor was now sanctioned by academia, which saw the introduction of a formal diploma and licensing to access career privileges and a new-found elevated social status based on a paternalistic system. The institution of health and medicine was born, and the physician became its leading expert and authoritative figure.
This transition made the patient a subordinate and passive actor when not exploited or experimented on in the name of scientific research.
In the mid-20th century, the physician-patient relationship was considered interactive, almost familiar. Whether people lived in rural or urban areas, most had a family doctor who had seen multiple generations go through life and would come to their house upon a phone call. Since then, the paternalistic approach has remained, and physicians can be authoritative, dismissive, downright disrespectful, or abusive.
But technology and the internet have brought yet another dynamic shift. E-health has revolutionized healthcare by organizing and disseminating an absurd breadth of information.
In the late 90s and early 2000s, websites curating medical information, symptomology, or the best doctor in one area changed the physician-patient interaction during consultation.
They morphed patients into consumers while the healthcare industry had already begun to monetize its services, medication, and research disruptively.
Today, about half of the patients in the U.S. seek relevant information online before consulting their primary doctor, and more than two-thirds discuss their findings during consultations (Tan et al., 2017).
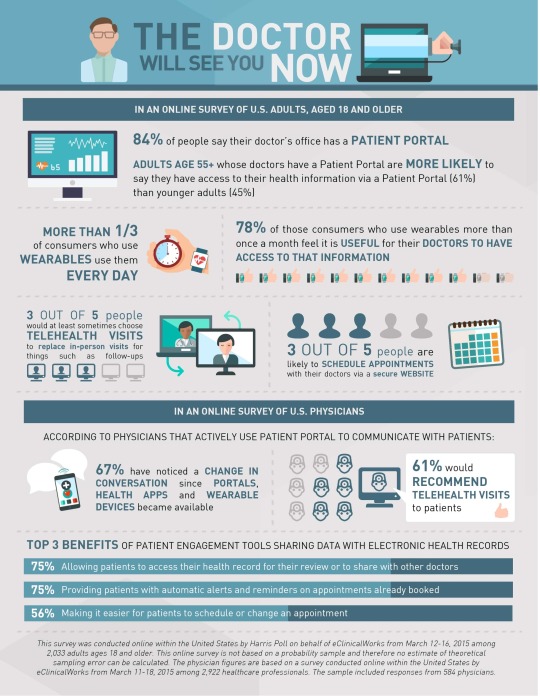
In the 20th century alone, we saw the introduction of the Electronic Patient Record, Telehealth, electronic wearables, and the E-Health Expert Patient. However, looking back on the history of health and medicine, that relationship was not always exclusive. This presentation explores how knowledge and innovation have continually transformed the physician-patient relationship and deconstructs the nostalgic rhetoric about this bonded interaction that has not always existed.
0 notes
Text
An Abbreviated and Simplified History of Medicine and the Physician Role
30 000 BCE: Cave paintings from almost 30,000 years ago show scenes of medicine people and community members participating in healing ceremonies and exchanging medicinal plants.
Let us remember that mental and physical affliction was always related to sacred beliefs and caused by the power of divinities. At the time, medicine people used magic and herbal potions to cure demons' spells.
3000-2000 BCE: The Sumerians, considered the first organized widespread civilization, reported detailed surgical procedures, medicinal plant prescriptions, and exorcism on clay tablets from 3000 to 2000 BCE.
Of importance, history reveals that women were surgeons and doctoresse since 3500 BCE, especially in Egypt, Italy, and Greece. During the antiquity and the development of the Greek civilization, we see the emergence of the rational and scientific method to push back against the supernatural. Many Greek thinkers were inspired by the ancient Egyptian civilization, who left behind knowledge about many healing agents.
1500 BCE: Ancient Indian Medicine was centered around Ayurvedic practices, based on a sacred Hinduist text, The Atharvaveda. Traditional Chinese Medicine is based on acupuncture, herbal mixtures, and other therapies practiced for thousands of years. However, the golden age of medicine started with the Zhou dynasty and was shaped by Taoist healing practices. Note that women were well-respected priests and healers at the time.
1100-146 BCE: The Ancient Greeks had a holistic approach to medicine and thought that environmental issues, trauma, and beliefs played a role in ailments, encompassed in the humoral theory. As the practice of trial and error took root, beliefs about divine punishment and grace were replaced by scientific theories based on biological cause and effect.
Doctors at the time actively preached that imbalances between the four humors: blood, phlegm, yellow bile, and black bile were responsible for illnesses. SES was also a concern as poor people were more afflicted by deplorable living conditions, giving rise to injuries, sanitary-related diseases, and famine.
440-360 BCE: Hippocrates, considered the foundational figure of modern medicine, established the first medical school at Cos and began to document different illnesses with his apprentices. They created medical terminology and drafted the first binding document of ethics called the Hippocratic Oath.
It is still in use today and affirms that physicians must follow a set of guiding and ethical principles in caring for their patients. Other prominent Greek physicians who inspired modern medicine are Asclepius, Diocles of Carystus, and Praxagoras of Cos. Their lasting influence was felt on European and Islamic medicine until the 14th century. We should also note that Aristotle, one of the most influential philosophers from antiquity, was greatly concerned about empiricism in its ecological and natural environment and influenced the advancement of medicine at the time.
400-1453 CE: Byzantine Medicine built upon the medical knowledge of the Greco-Roman empire and compiled it into textbooks. Islamist physicians became experts in anatomy, ophthalmology, pharmacology, pharmacy, physiology, and surgery, and their contributions and rigorous record-keeping pulled Europe out of the Dark Ages.
476-1450 CE: Unfortunately, during the Middle Ages and the rise of the male-dominated clergy, women were forbidden to practice surgery and medicine, among other things. However, in small pockets of Europe, between 100 CE and 1300 CE, cities like Bologna, Paris, and Oxford opened medical schools to teach rudimentary surgery and medicinal treatments. Students from wealthy families all over Europe would pursue academia for about eight years, three years of pre-med, and five years of medical school, which is relatively similar to today's curriculum's length without counting residency. Of note, a woman physician was awarded her degree in Sicily in 1376.
1600s: In Early Modern Medicine, in the 17th century, the civilian–physician ratio was still small, with a majority of unlicensed practitioners, of which 25% were women. Two key aspects that marked the Renaissance were the uptick in dissections, which fueled the advancement of anatomy and blood circulation understanding, and the microscope. Nuns played a fundamental role in hospitals and were the precursors of nurses in Catholic countries.
1700s: During the 18th century, the Age of Enlightenment, physicians became respected academics and saw a rise in social status.
1800s: The early 19th century marks the era of Late Modern Medicine and the rise in microbiology research to understand microorganisms like bacteria. New sanitary measures, like surgeons washing their hands thoroughly, were implemented, saving countless lives. Louis Pasteur and others introduced vaccines. Nursing schools opened in the late 19th century and became an attractive career for aristocratic and bourgeois women.
Elizabeth Blackwell was the first woman to earn a medical degree in 1849, but it was still challenging for women to become physicians in the United States until the 1970s.
0 notes
Text
The Contemporary Physician-Patient Relationship
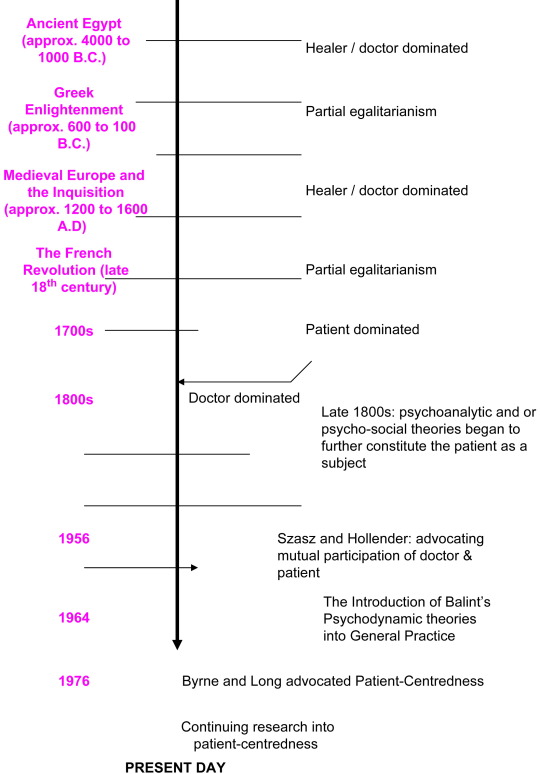
Kaba, Ra, and Prasanna Sooriakumaran. 2007. "The Evolution of the Doctor-Patient Relationship." International Journal of Surgery 5(1), 57–65. https://doi.org/10.1016/j.ijsu.2006.01.005
1950s-Present Day: The paternalistic model has dominated the landscape from the 19th century until today and lies in the foundational principle of the Hippocratic Oath, which asserts that physicians will do no harm and deliver expert treatment based on the beneficence criterion.
So, the doctor's role is to act in the patient's best interest. That role becomes overpowering and denies the patient's agency.
The psychoanalytic and psychosocial theories push for the evolution of this relationship and the redefinition of the patient's role. Those theories advocate for the physician to be more attentive to the patient's narrative and emotions. Self-agency is reintroduced as a means towards a more cooperative interaction during the consultation.
Thus, the embodiment of the patient into a sensible and sensitive individual brings the elements of empathy, trust, and reassurance and slightly shifts the power dynamic.
1960s: Later in the sixties, we see the emergence of the Therapeutic Alliance. The patient is 1) informed and understands the proposed treatment care plan, 2) asked to consent to the plan, and 3) the exchange between physician and patient is caring and empathetic.
0 notes
Text
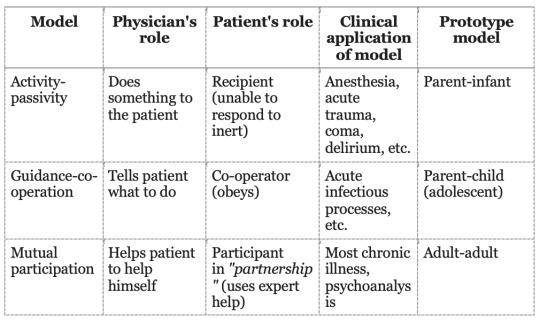
Szasz and Hollender (1956) propose three basic models of the doctor-patient relationship
0 notes
Text
Key Points about the Introduction of Systematic Information Ledgering and Organization
A few decades ago, you could call your doctor for a home visit. They would come to your house and give you a complete physical exam and prescribe treatment on the spot for most common ailments. There was a sense of familiarity because your physician had taken care of your grandparents, parents, and you as a child and maybe had overseen your pregnancy.
Today, there is a concerning scarcity of primary family doctors. Patients have to wait many months to see one.
Upon arrival, you fill out forms describing your symptoms, family history, and health insurance information. A nurse technician takes your vitals, and you have a quick discussion to explain your symptoms to your doctor, who will either write a script for common medication or send you to the appropriate specialist for extra testing like bloodwork or imaging.
There is no physical contact during the consultation, and the physician shows no interest in knowing you personally.
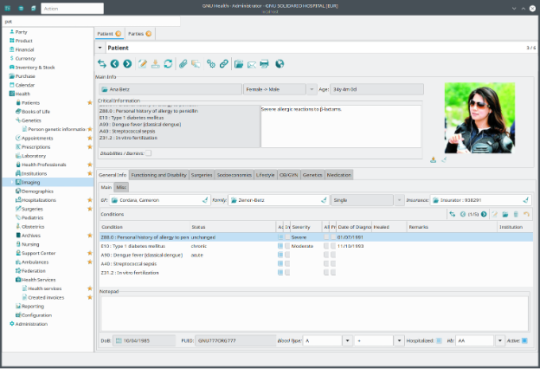
The front desk handles your chart from the doctor's notes. This is the product of many decades of transformation that led to a sanitized, systematic, and impersonal relational dynamic that began with the introduction of the Electronic Patient Record (EPR).
Physicians and patients used to interact more consistently when doctors used conversational techniques to assess the patient's overall state while taking notes on paper without interrupting eye contact and the patient narration.
Then came the Electronic Health Record (EHR), which required physicians to familiarize themselves with computers to keep records electronically in a centralized system.
It required a shift in attention and time away from the consultation.
Less eye contact and pointed questions made the conversation feel suspicious.
Questions became impersonal, unrelated to the symptoms of interest.
There was little room to build trust and patient adherence to treatments.
This marks the first disruption of modern innovation that will deteriorate the contemporary physician-patient relationship.
0 notes
Text
Displays of authority in the clinical consultation: A linguistic ethnographic study of the electronic patient record
JOURNAL ARTICLE #1
Swinglehurst, Deborah. 2014. "Displays of Authority in the Clinical Consultation: A Linguistic Ethnographic Study of the Electronic Patient Record." Social Science & Medicine 118(C), 17–26. https://doi.org/10.1016/j.socscimed.2014.07.045
The introduction of computers into general practice has changed the dynamics of clinical consultation, mainly through the widespread adoption of the electronic patient record (EPR) to support patient care. General practitioners spend about 40% of their consultation interacting with the computer (Kumarapeli and de Lusignan, 2013).
The attention devoted to electronically recording the patient's history and symptoms negates direct eye contact and organic human interaction.
"The EPR contributes to the display and circulation of authority in the consultation, using detailed analyses to illustrate how complex the consultation becomes when the EPR is integrated into it. The EPR creates new opportunities, including medication surveillance, prompts to health promotion, registration, recall, structured review of patients with chronic diseases, and complex risk calculations. It also places new demands on the consultation. It introduces new tensions, both in its contribution to the moment-by-moment unfolding of the interaction (the 'here and now') and through hosting and circulating new voices, constituting a "dilemma of attention" (Swinglehurst et al., 2011).
Researcher Swinglehurst argues that the EPR enhances the physician's authority by delivering new and complex data that is useful for the patient's overall care. However, the new computer system takes away from the immediate patient-physician interaction.
"Recent work on the use of electronic templates in the context of chronic disease management in general practice shows that their use may privilege 'hard' biomedical data over 'softer' more personal information" (Checkland et al., 2007; Rhodes et al., 2006, Rhodes et al., 2008, Swinglehurst et al., 2012).
Swinglehurst finds that the EPR demands specific kinds of data to be measured and evaluated by algorithms. This creates some tension as the patient has less room to share more narrative-driven and intimate details about their affliction, but cannot be formatted adequately for the EPR.
0 notes
Text
Key Points about the Disappearance of the Physical Exam
Doctors used to take your temperature, check your ears with an otoscope, look at your throat, listen to your lungs and heart with a stethoscope, check your gut health by performing abdominal tapping, and your joints health using a reflex hammer.
The introduction of electronic devices encouraged doctors to delegate those steps to nurse technicians.
This, in turn, increases patient turnover.
However, it also deteriorates the connection between patients and physicians.
There is no physical exam, which significantly diminishes touch, human interaction, and potentially the physician's ability to empathize. This, of course, happens in conjunction with the lack of familiarity and continuation with said patients.
The physical exam has always been an opportunity for doctors to demonstrate expertise with a show of tools and a way to ensure that the physician understands precisely what requires their attention after further physical investigation.
There is no opportunity to discover other issues outside of patient awareness.
The doctor cannot reevaluate the patient's presentation of symptoms.
It is also a way for the patient to evaluate trust as the physician touches the patient with calm expertise and without crossing boundaries. A physician who acts with professionalism and asks for consent will foster trust and compliance over time.
0 notes
Text
The Disappearance of the Primary Care Physical Examination—Losing Touch
JOURNAL ARTICLE #2
Hyman, Paul. 2020. "The Disappearance of the Primary Care Physical Examination—Losing Touch." JAMA Internal Medicine 180(11), 1417–1418. https://doi.org/10.1001/jamainternmed.2020.3546
"As our primary care practice has pivoted to telehealth and the physical examination has been ripped away from me, I find myself reflecting on what value the examination has. It is clearly needed at times to make a diagnosis."
- MD Paul Hyman has been practicing for 15 years, and the physical examination has always been integral to his interaction with patients.
"What was less apparent to me before the pandemic was how a thorough physical examination provides a measure of objectivity that can help me rethink a patient's narrative. When patients and I disagree on a plan, the physical examination not only provides data but also acts as an arbiter. For instance, patients sometimes feel a need to use antibiotics to treat a respiratory infection. If I communicate that results of their lung examination are clear and that their oxygen saturation levels are normal, they often feel more reassured that they do not need medication."
- Doctor Hyman argues that the physical examination provides an objective and physical assessment of the patient that he can use to assert his expertise and provide reassurance.
"In an admission of my insecurity, the physical examination remains one of the few domains where I maintain a sense of professional skill and authority. I have never been much of a proceduralist. The mainstay of what I offer to patients is the ability to listen to them, to use critical thinking skills, and to offer my knowledge and experience. But those skills are sometimes challenged in a world where patients research their own health and develop their own medical narratives. The physical examination remains a place where I offer something of distinct value that is appreciated."
Finally, Hyman admits that in the era of WebMD, the physical examination is the last refuge for bringing expert evidence against patients' self-diagnoses and creating a connection, a dialogue.
0 notes
Text
Key Points about the Reconfiguration of the Physician-Patient Consultation Caused by the Proliferation of E-Health Information
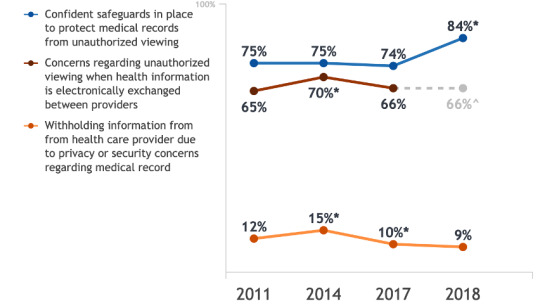
The proliferation of internet health information about symptomology, causes of illnesses, and potential treatments have, in some way, caused patients to feel more knowledgeable and empowered about their medical concerns.
The patient comes in prepared with pointed questions about their initial self-assessment before considering sharing their actual symptoms.
Physicians have to engage with patients to understand their actual symptoms and parse out the validity and credibility of the material they bring forth.
This creates tension because patients come in during their consultation with preconceived ideas about their medical issues. At the same time, doctors have to debate concerns that may not even be relevant to the patient's ailments.
Some doctors, similarly with using the EPR, complain that this effort consumes precious consultation time.
They lament the anxiety that some of the online searches create in their patients.
Physicians generally don't want to spend extra time answering emails to approve or disprove internet sources or alternative treatments and engage further with their patients outside of the consultation.
Patients will use different tactics to bring up their online search findings.
There are gender differences in disclosure. Men feel more confident about sharing their findings. At the same time, women are more apprehensive and often mention the resilient paternalistic approach that encourages doctors to be dismissive regardless of the quality of the online material.
Patients who receive dismissive feedback from their doctors feel incredibly dissatisfied. In the worst cases, patients and physicians argue over different concerns, usually ending with the patient discontinuing their relationship with their physicians.
Other physicians welcome this more cooperative interaction and seem to gain in patient adherence.
Some physicians will ask their patients about what they found and encourage them to evaluate the information critically. This attitude fosters mutual respect and trust.
0 notes
Text
"How online searches fuel health anxiety: Investigating the link between health-related searches, health anxiety, and future intention."
CRITICAL REVIEW #1
Peng, Rachel X. 2022. "How Online Searches Fuel Health Anxiety: Investigating the Link between Health-Related Searches, Health Anxiety, and Future Intention." Computers in Human Behavior, 136, 107384. https://doi.org/10.1016/j.chb.2022.107384
Findings
- The study found that the relationship between information overload and illness likelihood and body vigilance is significant, as well as the relationship between information quality and catastrophic misinterpretation.
- Information conflict also significantly influences illness likelihood, catastrophic misinterpretation, and information processing bias.
- Regarding future behaviors, the study found that body vigilance and catastrophic misinterpretation had a significant relation to seeking healthcare and illness likelihood.
- Finally, self-efficacy significantly influences illness likelihood related to e-health searching.
Peng's study critically assesses potential patients' mental state and newly acquired related behaviors before they see their primary healthcare provider.
Those findings demonstrate that patients may go to their appointments with heightened anxiety, misinformation, and persistent beliefs about false diagnoses.
This may represent a potential challenge for physicians facing trust and patient nonadherence difficulties. Doctors have to face patient's scrutiny about their expertise and help the patient dissipate their worry about a diagnosis that may not even apply to them and should impact the patient-physician relationship.
0 notes