Text
WHAT IS TAVI ?
Share
Transcatheter Aortic Valve Replacement is a process conducted very nominally to replace a firm aortic valve that cannot open. It has to be replaced because if the aortic valve cannot open, it diminishes the blood flow from the heart to the body. This procedure is required to prevent aortic stenosis which causes risky symptoms like chest pain, breathlessness, etc.
Note : Cardium is the best cardiology center led by a leading Cardiologist in Mumbai, Dr. Rahul Gupta, who has helped many patients get treated with TAVI and TAVR in Mumbai and Pan India. If you are searching for a TAVI Doctor, feel free to connect with us.
Who and why would patient need to option for TAVI ?
The aortic valve is one of the four valves in our heart. The valves open and closes, allowing the flow of blood from one chamber to another and later to the entire body. The person who has a problem with their aortic valve and has a high risk of open-heart surgery are good candidates for TAVI.
Transcatheter Aortic Valve Replacement is recommended to patients who suffer from Aortic Stenosis. Aortic Stenosis is a condition where the opening of the heart's aortic valve is narrowed. This prevents blood flow from the heart to the aorta, then to the other parts of the body since the condition does not allow the heart to open completely. Even though AVS can range from mild to severe, symptoms develop when this condition worsens.
The symptoms include severe chest pain, shortness of breath, rapid increase in heart pulse, and fatigue. If not treated on time, it can even lead to heart failure. Although there are certain medications to treat this condition, proper surgery to replace the aortic valve is the only way through which it can be prevented. Some specialists recommend patients to go through open-heart valve surgery when diagnosed with AVS but in some cases, this surgery can cause further pain in the patient's chest. So, in cases like these, Transcatheter Aortic Valve Replacement is recommended because it can reduce shortness of breath and the risk of heart failure.
How is TAVI procedure conducted ?
TAVI is a surgical procedure performed in an operation theatre. It involves the implantation of new valves made from animal tissues without removing the old and damaged valves. It a beneficiary option for patients who require valve replacement without undergoing massive open-heart surgery.
This surgery is performed via a very small opening, leaving the rest of the chest bones and muscles unaffected.
There are two approaches for performing the surgery. The doctor chooses the best suitable method depending on the patient’s condition and diagnosis
Transapical Approach - Via making a small incision in the chest and entering through the largest artery or the apex of the left auricle.
Transfemoral Approach - Entering the through femoral artery without requiring any surgical incision in the chest.
Read more…
Subscribe now
0 notes
Photo
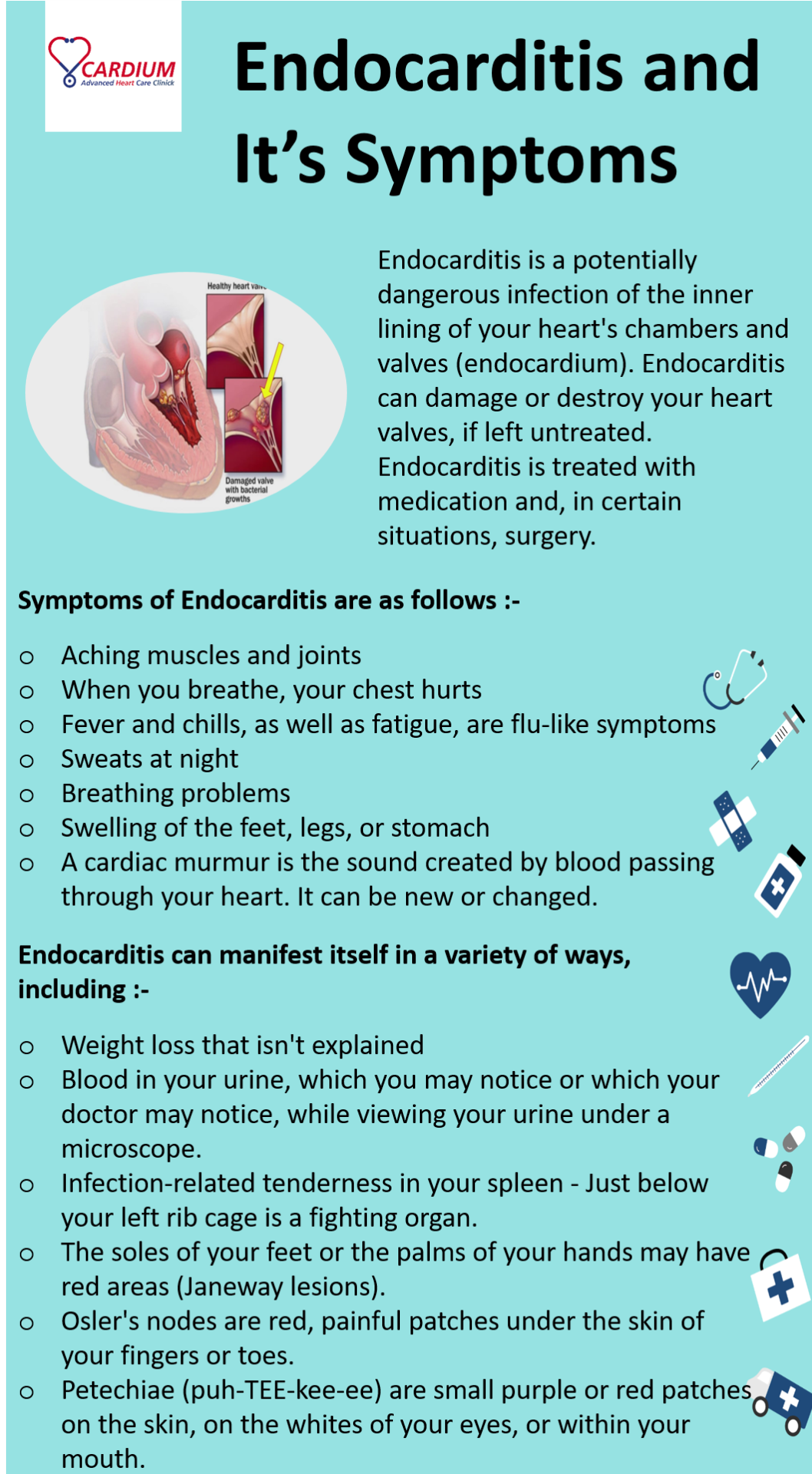
In this Infographic, we have told you, what is endocarditis and what are its symptoms.
If you want to know about other heart threatening diseases, please click the link below,
https://www.cardium.in/heart-diseases.php
#bestcardiologistinnavimumbai#cardiologistinnavimumbai#heartcareclinic#heartspecialistinnavimumbai#besthearthospitalinnavimumbai#endocarditis
0 notes
Text
Complete Information about Pericarditis
What is Pericarditis ?
Pericarditis is a condition in which the thin, saclike tissue that surrounds the heart becomes inflamed and swollen (pericardium). Sharp chest pain is a common pericarditis symptom. The pericardium's inflamed layers press against one other, creating chest pain. Pericarditis is typically minor and self-resolving. More severe cases may be treated with medication or, in rare occasions, surgery. Early detection and treatment of pericarditis can assist to lower the risk of long-term consequences.
Symptoms :
The most common pericarditis symptom is chest discomfort. It has a sharp or stabbing sensation most of the time. Some patients, however, experience dull, achy, or pressure-like chest pain. Pain from pericarditis is most commonly felt behind the breastbone or on the left side of the chest.
The discomfort could be caused by :
The left shoulder and neck are affected.
Coughing, reclining down, or taking a big breath make it worse.
Improve your sitting or leaning forward skills.
Pericarditis can also cause the following signs and symptoms :
Cough
Fatigue, a general feeling of weakness, or being ill are all symptoms of being unwell
Swelling of the legs
Fever of a low intensity
Heart pounding or racing (heart palpitations)
You may have shortness of breath while lying down
The stomach swells (abdomen)
The symptoms of pericarditis vary depending on the type. Pericarditis is divided into different categories based on the pattern of symptoms and the length of time that they last.
Acute pericarditis is a type of pericarditis that develops quickly and lasts for three weeks or less. Future episodes are possible. It can be difficult to tell the difference between acute pericarditis and pain after a heart attack.
After an acute pericarditis episode, recurrent pericarditis develops four to six weeks later, with no symptoms in the interim.
Persistent pericarditis usually lasts four to six weeks, but no longer than three months. The signs and symptoms do not stop.
Chronic constrictive pericarditis has a slow start and lasts for more than three months.
When should you see a doctor ?
If you acquire new chest discomfort symptoms, seek medical attention right once.
Pericarditis has several symptoms that are similar to those of other heart and lung diseases. If you experience any form of chest pain, it's critical to see a doctor for a comprehensive examination.
Causes :
Pericarditis is notoriously difficult to diagnose. It's possible that no reason has been discovered (idiopathic pericarditis).
Pericarditis can be brought on by a number of things, including :
After a heart attack or heart surgery, the immune system responds to the damage to the heart (Dressler syndrome, also called postmyocardial infarction syndrome or postcardiac injury syndrome)
COVID-19, for example, is an infection.
Lupus and rheumatoid arthritis are examples of inflammatory diseases.
A heart or chest injury is a serious condition that requires immediate medical attention.
Kidney failure and cancer are two more chronic health issues.
Complications :
Pericarditis can be diagnosed and treated early, which minimizes the risk of consequences. Pericarditis can lead to the following complications :
A accumulation of fluid around the heart (pericardial effusion) - Further heart issues may result from the fluid buildup.
The lining of the heart thickens and scars (constrictive pericarditis) - Long-term pericarditis can cause chronic thickening and scarring of the pericardium in certain persons. The alterations make it impossible for the heart to fill and empty properly. Severe swelling of the legs and abdomen, as well as shortness of breath, are common symptoms of this rare consequence.
Fluid buildup puts pressure on the heart (cardiac tamponade) - This potentially fatal disease stops the heart from adequately filling. Blood pressure drops dramatically when less blood leaves the heart. Cardiac tamponade necessitates immediate medical attention.
Prevention :
Pericarditis does not have a specific treatment. Taking the following precautions to prevent infections, on the other hand, may assist to minimize the risk of heart inflammation :
Until they've recovered, stay away from folks who have a viral or flu-like sickness - If you have symptoms of a viral infection, try to stay away from others.
Maintain a healthy level of hygiene - Hand washing on a regular basis can help prevent the spread of sickness.
Vaccines are highly recommended - Maintain current vaccinations, including those that protect against COVID-19, rubella, and influenza, all of which can cause myocarditis. Rarely, the COVID-19 vaccine can induce pericarditis (inflammation of the outer heart lining) and heart muscle inflammation, especially in males aged 12 to 17. Consult your doctor about the advantages and disadvantages of immunizations.
Diagnosis :
A health care practitioner would usually examine you and ask questions about your symptoms and medical history to diagnose pericarditis.
To listen to heart sounds, a stethoscope is usually placed on the chest and back. A pericardial rub is a sound produced by pericarditis. When the two layers of the sac enclosing the heart (pericardium) brush against each other, a noise is produced.
Typically, blood tests are performed to look for indicators of a heart attack, inflammation, or infection. Other tests for pericarditis diagnosis include :
Electrocardiogram (ECG)
An electrocardiogram (ECG) is a painless and rapid examination that records electrical signals in the heart. A monitor is connected to sticky patches (electrodes) with wires attached. They keep track of the electrical impulses that cause the heart to beat. The data is stored in a computer and displayed as waves on a monitor or on paper.
Chest X-ray
An X-ray of the chest can reveal changes in the size and shape of the heart. It can aid in the detection of an enlarged heart.
Echocardiogram
Ultrasound waves create images of the beating heart. An echocardiography can reveal how effectively the heart pumps blood and whether fluid has accumulated in the tissue surrounding the heart.
Computerized tomography (CT) scan of the heart
X-rays are used to create pictures of the heart and chest in cardiac CT scans. The test can detect cardiac thickening, which could indicate constrictive pericarditis.
Magnetic resonance imaging of the heart (MRI)
Cardiac MRI creates cross-sectional images of the heart using a magnetic field and radio waves. An MRI examination of the thin tissue surrounding the heart can indicate thickening, inflammation, or other alterations.
Treatment :
Treatment for pericarditis is determined on the origin and degree of symptoms. Pericarditis that is mild may improve without treatment.
Medications
Anti-inflammatories and anti-swelling medications are frequently administered. Here are several examples:
a) Pain relievers
Pain from pericarditis is commonly managed with over-the-counter analgesics such aspirin or ibuprofen (Advil, Motrin IB, others). Pain medications with a prescription strength are also an option.
b) Colchicine (Colcrys, Mitigare)
This medication works by reducing inflammation in the body. It's used to treat acute pericarditis and recurrent symptoms. If you have liver or renal illness, you should avoid taking this medication. Colchicine can also cause interactions with other medications. Before administering colchicine, your doctor will thoroughly examine your medical history.
c) Corticosteroids
Corticosteroids are powerful anti-inflammatory drugs. If pericarditis symptoms do not improve with previous drugs or if symptoms reappear, a corticosteroid such as prednisone may be recommended.
Antibiotics and, if necessary, drainage may be used to treat pericarditis caused by a bacterial infection.
Surgical treatments or other procedures
If pericarditis causes fluid to build up around the heart, the fluid may need to be drained through surgery or another method.
Pericarditis can be treated with surgery or other techniques such as:
a) Pericardiocentesis :
A sterile needle or a tiny tube (catheter) is used to extract and drain excess fluid from the pericardial cavity during this treatment.
b) The pericardium is removed (pericardiectomy) :
If the sac enclosing the heart is chronically stiff owing to constrictive pericarditis, the entire pericardium may need to be removed.
Home remedies and a healthy lifestyle
Rest and over-the-counter pain medications, given as instructed by your healthcare professional, may be all that's required for mild pericarditis.
Avoid excessive physical activity and competitive sports while you recover. Pericarditis symptoms might be triggered by such exercise. Inquire with your doctor about how long you should rest.
#bestcardiologistinnavimumbai#cardiologistinnavimumbai#heartspecialistinnavimumbai#besthearthospitalinnavimumbai#heartcareclinicinnavimumbai#heartdiseasetreatmentinnavimumbai
0 notes
Photo
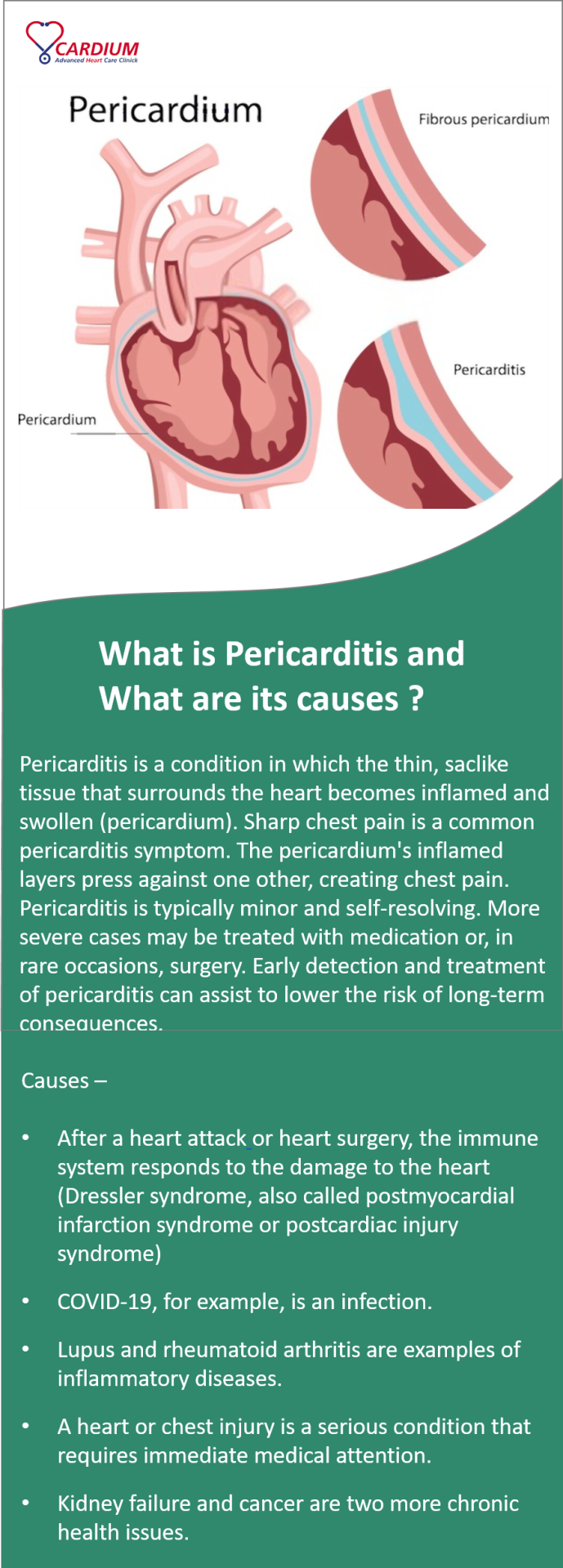
In this Infographic, we have told you, what pericarditis is and what causes pericarditis.
If you are interested to know about other heart threatening diseases, please click here.
#bestcardiologistinnavimumbai#cardiologistinmumbai#heartspecialistinnavimumbai#besthearthospitlainnavimumbai#heartcareclinicinnavimumbai#treatmentforpericarditisinnavimumbai
0 notes
Text
Rheumatic Heart Disease - One of the Danger Heart Disease

What is Rheumatic Heart Disease ?
In Rheumatic Heart Disease, rheumatic fever leads to permanent damage to the heart valves. Streptococcal infection can lead to damage to the heart valve if left untreated or under-treated for strep throat or scarlet fever. The immune response can cause an inflammatory condition in the body that can damage the running valve.
Causes of Rheumatic Heart Disease
➢ Rheumatic fever, an inflammatory condition that can affect numerous connective tissues, including the heart, joints, skin, and brain, causes rheumatic heart disease.
➢ The heart valves might become inflamed and scarred over time. This might cause the heart valve to constrict or leak, making regular heart function difficult. This might take years to show and ultimately result in heart failure.
➢ Rheumatic fever can strike anyone at any age, but it is most common in children aged 5 to 15. In industrialized countries such as the United States, it is uncommon.
Who is at Risk for Rheumatic Heart Disease ?
➢ Rheumatic heart disease can be exacerbated by untreated or undertreated strep infections.
➢ Rheumatic fever and rheumatic heart disease are more common in children who have repeated strep throat infections.
Symptoms of Rheumatic Heart Disease
The diagnosis of rheumatic heart disease requires a recent history of strep infection or rheumatic fever. Rheumatic fever symptoms vary and typically develop 1 to 6 weeks after a strep throat infection. The infection may have been too mild to be detected, or it may have disappeared by the time the person sees a doctor.
The following are the most prevalent rheumatic fever symptoms :
✓ Fever
✓ Joints that are swollen, sensitive, red, and exceedingly painful, especially the knees and ankles.
✓ Nodules are a type of nodule that is (lumps under the skin).
✓ A rash that is red, elevated, and lattice-like that appears on the chest, back, and belly.
✓ Shortness of breath and soreness in the chest.
✓ Uncontrolled arm, leg, or facial muscular movements
✓ Weakness
Rheumatic Heart Disease symptoms vary depending on the severity of valve damage and may include :
✓ Breathing problems (especially with activity or when lying down)
✓ Pain in the chest
✓ Swelling
Diagnosis of Rheumatic Heart Disease
A strep infection is common in people with rheumatic heart disease, and they may have had one lately. To check for strep, a throat culture or blood test may be done. During a regular physical examination, they may have a murmur or rub. The blood flowing around the damaged valve causes the murmur. When inflammatory cardiac tissues move or rub against each other, the rub occurs.
Tests used to identify rheumatic heart disease, in addition to a comprehensive medical history and physical examination, may include:
❑ Echocardiogram (Echo)
An echocardiogram is a test that examines the heart (echo). The chambers and valves of the heart are examined using sound waves. As an ultrasound transducer is run over the skin overlaying the heart, echo sound waves generate a picture on a screen. Damage to the valve flaps, blood backflow through a leaky valve, fluid around the heart, and cardiac enlargement can all be seen on an echo. It's the most effective test for detecting heart valve issues.
❑ Electrocardiogram (ECG)
This test measures the strength and timing of the heart's electrical activity. It can identify heart muscle injury and display irregular rhythms (arrhythmias or dysrhythmias). To detect electrical activity, little sensors are glued to your skin.
❑ Chest X-ray
To evaluate your lungs and discover if your heart is enlarged, an X-ray may be taken.
❑ Cardiac MRI
This is a heart imaging test that produces detailed images of the organ. It can be used to examine the heart valves and muscle in greater detail.
❑ Blood Tests Certain blood tests can be used to detect infection and inflammation.
Treatment of Rheumatic Heart Disease
➢ Treatment depends in large part on how much damage has been done to the heart valves. In severe cases, treatment may include surgery to replace or repair a badly damaged valve.
➢ The best treatment is to prevent rheumatic fever. Antibiotics can usually treat strep infections and keep rheumatic fever from developing. Anti-inflammatory drugs may be used to reduce inflammation and lower the risk of heart damage. Other medicines may be needed to manage heart failure.
➢ People who have had rheumatic fever are often given daily or monthly antibiotic treatments, possibly for life, to prevent recurrent infections and lower the risk of further heart damage. To reduce inflammation, aspirin, steroids, or non-steroidal medicines may be given.
Complications of Rheumatic Heart Disease
The following are Some of the Complications of Rheumatic Heart disease :
▪ Heart failure is a serious condition. This can be caused by a heart valve that is substantially constricted or leaking.
▪ Endocarditis caused by bacteria. This is an infection of the heart's inner lining that can occur when the heart valves have been compromised by rheumatic fever.
▪ Pregnancy and delivery complications caused by heart disease. Before becoming pregnant, women with rheumatic heart disease should speak with their doctor about their situation.
Prevention of Rheumatic Heart Disease
Preventing strep infections or treating them with antibiotics when they do occur can help to prevent rheumatic heart disease. Even if you feel better after a few days, it's critical to take antibiotics as prescribed and complete them as directed.
#cardiologistinnavimumbai#cardiologistinmumbai#heartspecialistinnavimumbai#besthearthospitalinnavimumbai#heartspecialisthospitalinnavimumbai#rheumaticheartdiseasetreatmentinnavimumbai#rheumaticheartdiseasetreatment
0 notes
Photo
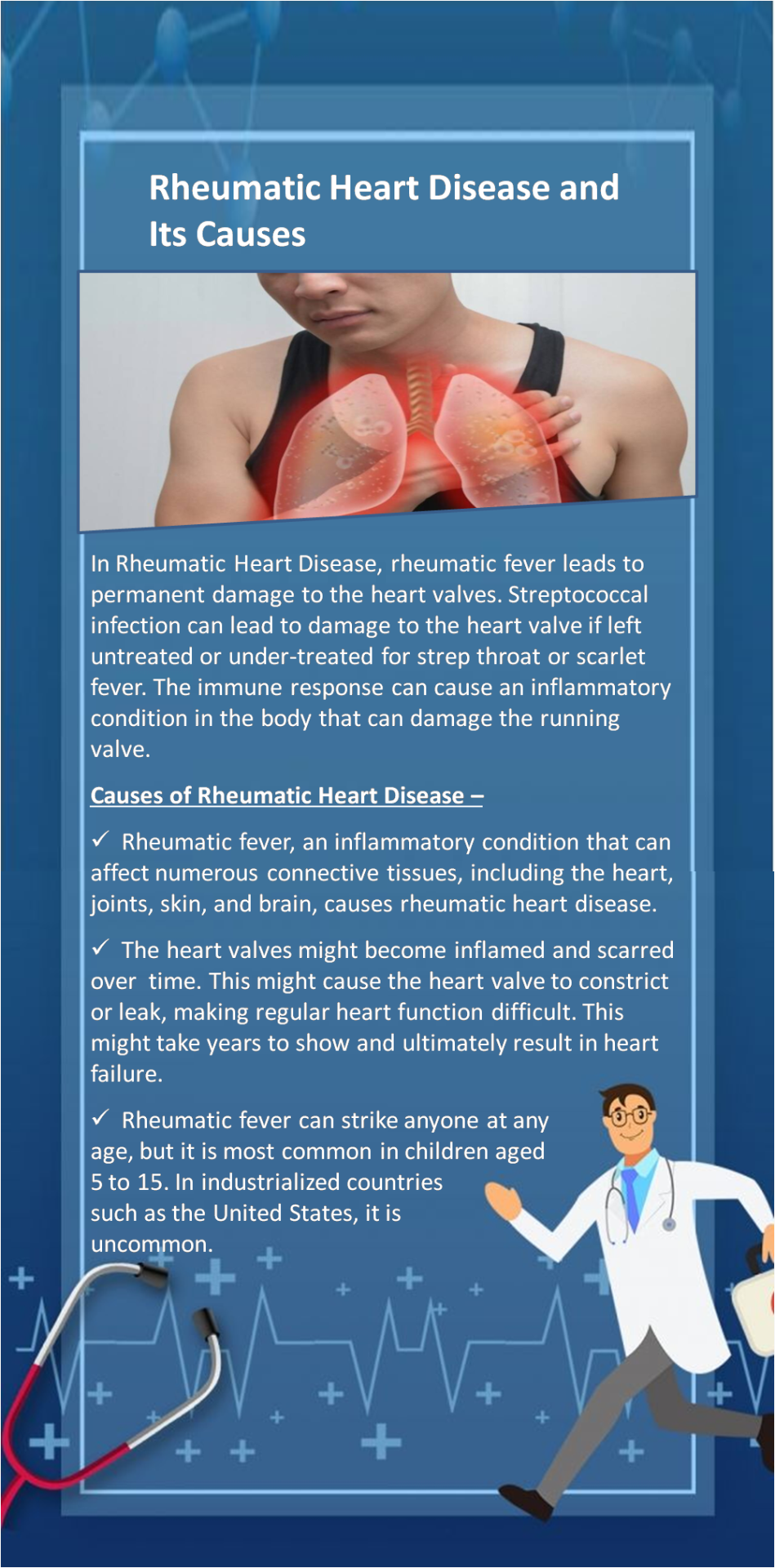
In this Infographic, we have explained to you What is Rheumatic Heart Disease, How this Disease poses a Risk to the Heart Valves, What are the Causes of this Disease, What can happen to your body, while this disease is occurring.
#bestcardiologistinnavimumbai#heartspecialistinnavimumbai#hearthospitalinnavimumbai#heartspecialisthospitalinnavimumbai#bestheartcareclinicinnavimumbai#cardiologistinmumbai#rheumaticheartdisease#rheumaticheartdiseasetreatment
0 notes
Text
Things No One Tells You About Heart Attack Recovery

Life is unpredictably unpredictable, but we can certainly forecast how our health will be in the future. Whatever we give our bodies now becomes their elixir for future survival. This emphasizes the need of paying close attention to what we eat and how we treat our bodies. The exponential rise in the number of deaths due to cardiac arrest is today's disguised wake-up call.
The majority of heart attacks are caused by the blockage of certain arteries. It cuts off the flow of blood, resulting in attacks. When a person returns home following heart surgery, they are more concerned about their heart's health. Cardiac rehabilitation, however, comes to their aid. It is a personalized program for patients that includes exercises and healthy eating habits to help them live healthier lives in the future.
How do you feel after a heart attack ?
Around one-fourth of patients report despair, rage, and dread after a heart attack. As people return to their normal routines, these natural reflexes fade. However, estimating the length of time, it will take is challenging.
You can do the following to help yourself feel better :
Get dressed and wake up every day.
Go for a walk every day rather than spending the entire day in bed. Regular exercise will keep your mind and body in good shape.
It's a good idea to resume hobbies and social activities that you enjoy.
Talk to family, friends, clergy, or a support group about your thoughts and feelings.
Have a good night's rest. Sleep deprivation can make you tired and irritable. You will have problems sleeping at night, if you sleep too much during the day.
Limit visits with friends and relatives at first to avoid becoming overtired. You can increase them depending on how you're feeling. These visits may aid in the gradual elevation of your emotions.
Join a heart attack recovery program - Emotional support is one of the numerous benefits of a supervised activity and education program. If you don't feel like your emotions are better or if you're worried about becoming depressed, the best thing you can do is, talk to your doctor. You can seek medication and counseling to help you get through this difficult time.
Diet
To avoid heart disease in the future, it's vital to consume a heart-healthy diet.
Six approaches for reducing the risk of coronary artery disease are listed below :
Increase your intake of fruits, vegetables, whole grains, and legumes.
Carefully select your fat calories.
Consume a wide range of foods containing the proper quantity of protein.
Reduce your cholesterol intake by eating a low-cholesterol diet.
Reduce your intake of simple carbohydrates and rely on complex carbohydrates for energy instead.
Reduce your salt intake while increasing potassium, magnesium, and calcium.
How can you keep a heart attack from happening again ?
The goal after a heart attack is to keep your heart healthy and reduce your risks to prevent further heart damage. Take your medications exactly as directed. Medication is given to the patient after he or she has undergone heart attack rehabilitation.
In the future, avoid blood clots.
Reduce the amount of effort required of your heart.
Improve your heart's function and recuperation.
Reduce cholesterol levels.
More medications may be supplied if necessary. Among these are medications for irregular heartbeats, blood pressure control, angina (chest pain), and heart failure. It's important not to rush your recovery after a heart attack because it could take months.
Recovery
During your heart attack rehabilitation, you'll receive guidance and support from a range of healthcare specialists, including :
Nurses
Physiotherapists
Dietitians
Pharmacists
Experts in physical activity
These medical professionals will help you recuperate safely and effectively, both physically and mentally. The rehabilitation procedure is usually divided into stages, with the first being a stay in the hospital, where your condition can be monitored and your future needs assessed. After being released from the hospital, you can continue your recovery at home.
The two most important goals of the rehabilitation process are as follows :-
Returning to your everyday routines after progressively regaining physical condition (known as cardiac rehabilitation)
Assist in reducing your risks of suffering another heart attack.
Exercise
When you arrive home, it's usually better to unwind and do only light exercises like walking up and down the stairs many times a day or taking a short walk.
Increase the amount of activity you do each day over several weeks. The state of your heart and overall health will affect how quickly you can accomplish this.
Your doctor may make more precise recommendations about how to increase your exercise levels.
Your heart attack rehabilitation program should include a variety of activities, depending on your age and abilities.
The majority of the exercises will be aerobic. These are designed to strengthen your heart, improve your circulation, and lower your blood pressure.
Aerobic workouts include cycling on an exercise bike, walking on a treadmill, and swimming.
Conclusion
Anyone who has had a heart attack faces unique concerns and challenges, and any advice or assistance you receive will be tailored to your situation. There are numerous local and national cardiac support groups where you can meet people who have gone through similar situations.
#bestcardiologistinnavimumbai#cardiologistinmumbai#heartattackrecoverytreatmentinnavimumbai#heartattacktreatmentinnavimumbai#heartdiseasetreatmentinnavimumbai#heartspecialistinnavimumbai#heartspecialisthospitalinnavimumbai
0 notes
Photo
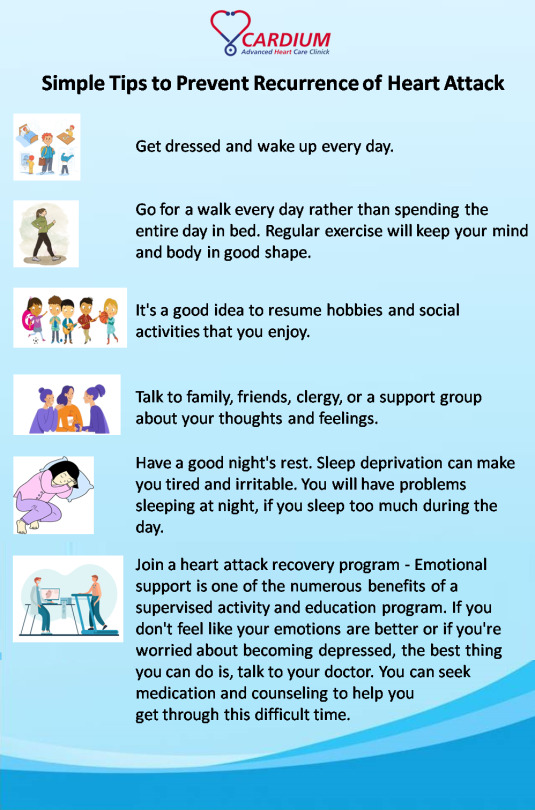
In this infographic, we have given you 6 simple tips that if you follow, you will stay away from any heart disease or heart attack. There are things that can be done easily in our daily life, so everyone can do it easily.
#bestcardiologistinnavimumbai#cardiologistinnavimumbai#heartspecialistinnavimumbai#heartcareclinic#besthearthospitalinnavimumbai#heartattacktreatmentinnavimumbai
0 notes
Text
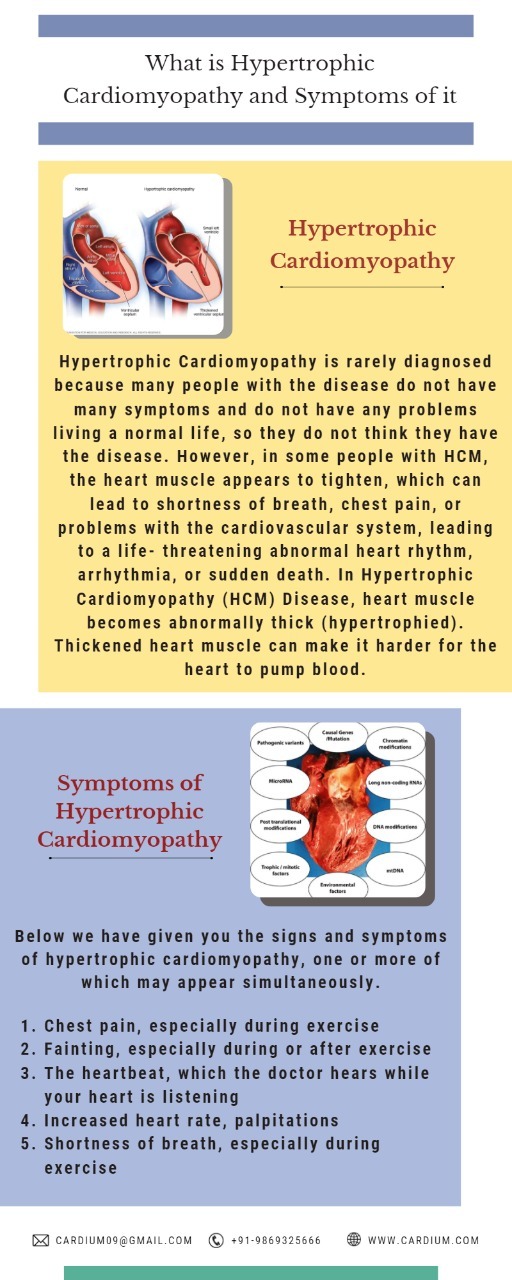
Important Information about Hypertrophic Cardiomyopathy
What is Hypertrophic Cardiomyopathy ?
Hypertrophic Cardiomyopathy is rarely diagnosed because many people with the disease do not have many symptoms and do not have any problems living a normal life, so they do not think they have the disease. However, in some people with HCM, the heart muscle appears to tighten, which can lead to shortness of breath, chest pain, or problems with the cardiovascular system, leading to a life- threatening abnormal heart rhythm, arrhythmia, or sudden death.
In Hypertrophic Cardiomyopathy (HCM) Disease, heart muscle becomes abnormally thick (hypertrophied). Thickened heart muscle can make it harder for the heart to pump blood.
Symptoms of Hypertrophic Cardiomyopathy
Below we have given you the signs and symptoms of hypertrophic cardiomyopathy, one or more of which may appear simultaneously.
Chest pain, especially during exercise
Fainting, especially during or after exercise
The heartbeat, which the doctor hears while your heart is listening
Increased heart rate, palpitations
Shortness of breath, especially during exercise
When to go to the doctor
Shortness of breath and palpitations can occur for a number of reasons. Therefore, it is important to make an accurate diagnosis immediately and take proper care of it. If you have a family history of HCM or any symptoms related to hypertrophic cardiomyopathy, you should see your doctor immediately.
If you experience any of the following symptoms for more than a few minutes, be sure to call 911 or your local emergency number.
1. Fast or irregular heartbeat
2. Difficulty breathing
3. Chest pain
Causes of Hypertrophic Cardiomyopathy -
1. The most common cause of hypertrophic cardiomyopathy is an abnormal gene mutation. This causes the heart muscle to become unusually thick.
2. In most people with hypertrophic cardiomyopathy, the muscle wall (septum) between the two lower chambers of the heart is thicker than normal. As a result, this thick wall can block blood flow to the heart. This is called obstructive hypertrophic cardiomyopathy.
3. If there is no significant obstruction to blood flow. The condition is called non-obstructive hypertrophic cardiomyopathy. This can cause stiffening of the main pumping chamber (left ventricle) of the heart. This prevents the heart from relaxing easily and therefore reduces the amount of blood that can be sent to the body by holding the ventricle in each heartbeat.
4. Patients with hypertrophic cardiomyopathy also have an abnormal arrangement of heart muscle cells called myofiber disorders. This can lead to arrhythmias in some patients.
Risk Factors -
Hypertrophic cardiomyopathy is usually passed down from family to generation.
If anyone in your household has hypertrophic cardiomyopathy, you have a 50% chance of developing the disease genetically.
Parents or relatives of a person with hypertrophic cardiomyopathy should ask their doctor for a diagnosis.
Complications -
Most patients with hypertrophic cardiomyopathy (HCM) do not have HCM-related health problems. But in the complications of hypertrophic cardiomyopathy, it appears to be one of the causes.
1. Atrial fibrillation - Thick heart muscle, as well as abnormal structure of heart cells, causes changes in the electrical system of the heart. As a result, the heart beats faster or irregularly. Atrial fibrillation can cause a stroke in your brain, which can lead to blood clots.
2. Blood flow blocked - In most patients, tightening of the heart muscle prevents blood from flowing out of the heart, leading to shortness of breath, chest pain, dizziness, and fainting.
3. Mitral valve problems - Thickening of the heart muscle prevents blood flow from the heart. As a result, the mitral valve between the left atrium and the left ventricle does not close properly. This results in no blood flow to the left atrium (mitral valve regurgitation), leading to worse symptoms.
4. Dialated cardiomyopathy - In very few patients with HCM, the thick heart muscle becomes weak and ineffective. As a result, the ventricle becomes enlarged and dilates, thus reducing its pumping capacity.
5. Heart failure - The constricted heart muscle can eventually become very stiff, so the heart can effectively fill with blood. As a result, your heart cannot pump enough blood to meet your body's needs.
6. Sudden heart attack death - Rarely, hypertrophic cardiomyopathy can lead to sudden cardiac death in patients of all ages. Most people with hypertrophic cardiomyopathy do not know they have the disease. Sudden death from a heart attack can be part of the problem of hypertrophic cardiomyopathy. This can happen in the case of high school athletes, other young, active adults as well as even healthy young people.
Prevention -
No restrictions for hypertrophic cardiomyopathy have been reported. However, it is important to identify the condition as soon as possible, so that the disease can be treated and thus avoid complications during treatment.
If your first-degree relative - parent, or other close relative has hypertrophic cardiomyopathy, the doctor may ask you to have a genetic test to diagnose the disease.
However, not everyone with HCM currently has a mutable detectable mutation. Also, some insurance companies may not cover the entire cost of genetic testing.
If a genetic test is not performed, or the results are not helpful. Your doctor may ask you to have a power echocardiogram test, if your family member has hypertrophic cardiomyopathy. Adolescent and competitive athletes must be screened once a year. For those who do not participate in adult athletics, it is better to check every five years.
#heartdiseasetreatmentinnavimumbai#treatmentforhypertrophiccardiomyopathyinnavimumbai#cardiologistinnavimumbai#bestcardiologistinmumbai#hearthospitalinmumbai#heartspecialisthospitalinmumbai#topcardiologistinmumbai
0 notes
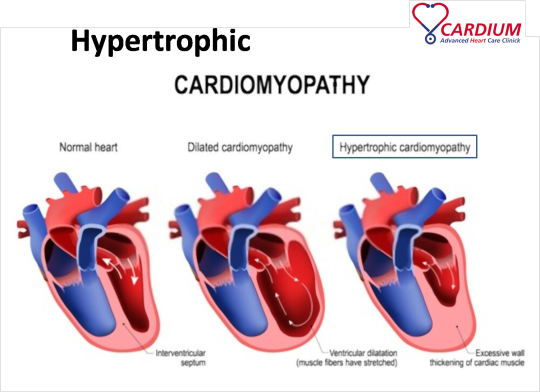
Photo
In this Infographic, we have explained to you what Hypertrophic Cardiomyopathy means, and you will know what dangerous conditions you have to face due to this disease, which can sometimes lead to death. We have also told you here, what are the symptoms of this disease and what are the important symptoms.
If you want to know the detailed information about Cardiomyopathy, please click the link below,
www.cardium.in/cardiomyopathy.php
#cardiologistinnavimumbai#cardiologistinmumbai#bestcardiologistinmumbai#hearthospitalinmumbai#besthearthospitalinmumbai#topcardiologistinmumbai#bestheardiseasetreatmentinavimumbai
0 notes
Photo

In this, we have given you information about what is inflammatory bowel disease (IBD), what are its types, how dangerous is this disease, how much and how it affects your body, what are the side effects of this disease.
If the disease is not treated in time, it can lead to ischemic heart disease.
You can read the information about ischemic heart disease here, www.cardium.in/heart-diseases.php
#cardiologistinnavimumbai#bestcardiologistinnavimumbai#besthearthospitalinnavimumbai#heartspecialistinmumbai#heartdiseasetreatmentinnavimumbai
0 notes
Text
Complete Information about Inflammatory Bowel Disease

A. What is Inflammatory Bowel Disease (IBD) ?
Inflammatory bowel disease, commonly known as IBD is a collection of diseases that generate chronic inflammation which includes pain and swelling in the intestines. IBD includes Crohn’s disease and ulcerative colitis. Both types of IBD affect the digestive system. Treatments can help to manage this lifelong condition.
Inflammatory bowel disease should be treated in time, otherwise it increases the risk of ischemic heart disease.
B. Types of IBD
There are mainly two types of IBDs, namely, Crohn’s Disease and Ulcerative Colitis.
1. Crohn’s Disease - It affects any part of the Gastrointestinal tract (from mouth to anus). Generally, it affects the portion of the smallintestine before the large intestine. All infected areas appear in patches that are immediately next to areas of healthy tissue. An inflammation reaches through the multiple layers of the walls of the Gastrointestinal tract.
2. Ulcerative Colitis - It occurs in the large intestine/colon and the rectum. Infected areas are continuous and not patchy. It usually starts at the rectum and spreads further into the colon. Inflammation is present only in the inner layers of the lining of the colon.
C. What are the symptoms of IBD ?
Inflammatory bowel disease symptoms differ, depending on the harshness of inflammation and where it occurs in the body. Symptoms might range from mild to severe. You're most likely to have periods of active illness followed by periods of remission.
Some common symptoms of IBD are as follows –
1. Persistent Diarrhoea
2. Abdominal Pain
3. Bloody Stools
4. Weight Loss
5. Fatigue.
6. Gas and Bloating.
Some rare symptoms of IND are as follows –
1. Fever
2. Itchy, red, painful eyes
3. Joint Pen
4. Nausea and Vomiting
5. Skin rashes and sores.
6. Vision Problems.
D. What causes IBD ?
Researchers / Scientists are still trying to determine why some people of IBD.
But here are some factors which play a key role –
1. Genetics
1 out of every 4 people with IBD has a family history of the given disease.
2. Response of Immune System
The immune system generally fights off infections. In people with IBD, the immune system mistakes foods as alien substances. It releases antibodies (proteins) to battle off this danger of IBD, causing IBD symptoms.
3. Environmental Triggers
People with a long family history of IBD may elaborate on the disease after exposure to an environmental trigger. These triggers contain smoking, stress, drug use, and depression.
E. How can Inflammatory Bowel Disease be cured ?
The doctor makes the diagnosis of inflammatory bowel diseases based on the systems and various exams and tests.
1. Stool Exam
You will be questioned for a stool sampling that will be transferred to a laboratory to rule out the possibility of bacterial, viral, or parasitic causes of diarrhea. In addition, the stool will be examined for traces of blood that cannot be seen with the bare nakedeye.
2. Blood Count
A nurse or lab technician will draw blood, which will also be sampled in the lab. An increment in the white blood cell count suggests the presence of inflammation. And if you have severe bleeding, the red blood cell count and hemoglobin degree may dwindle.
3. Other Blood Tests
Electrolytes such as sodium and potassium, protein, and inflammation markers, similar to Erythrocyte Sedimentation Rate (ESR) and C-reactive protein (CRP), maybe pictured to have a glance at how serious the disorder is. Perinuclear antineutrophil cytoplasmic antibody (pANCA) situations may be up in ulcerative colitis. In addition, specific tests for sexually transmitted complications may be done.
4. Barium X-Ray
Although seldom used, it can conform to the upper gastrointestinal (GI) tract-- the esophagus, abdomen, and small intestine-- for anomalies caused by Crohn's disease. You swallow a chalky white solution that coats the intestinal tract so it'll be observable onX-rays. Still, you'll be given an enema containing barium and asked to hold it in whileX-rays are taken of the rectum and colon If a barium x-ray is used to check the lower GI tract. Abnormalities caused by either Crohn's disease or ulcerative colitis may be shown up in theseX-rays.
5. Sigmoidoscopy
In this process, a doctor uses a sigmoidoscope, a slim, adjustable tube with a camera and light, to visually examine the last one-third of your large intestine, which involves the rectum and the sigmoid colon. The sigmoidoscope is fitted through the anus and the intestinal wall is visually examined for ulcers, inflammation, and bleeding. The doctor may also take biopsies of the intestinal filling with an instrument fitted through the tube. These will also be examined in a laboratory under a microscope.
6. Capsule Endoscopy
This test may be helpful to diagnose complications in the small intestine, similar to Crohn's disease. You ingest a small capsule that has a camera in it. Pictures are taken of the esophagus, abdomen, and small bowel and also transferred to a receiver you wear on a belt. The pictures are downloaded from the receiver onto a computer at the end of the process. The camera is transferred through your body into the washroom.
F. What are the distinguishable factors between irritable bowel syndrome (IBS) and inflammatory bowel disease (IBD) ?
The basic difference between IBD and IBS is that IBS is a syndrome or group of symptoms. The causes, symptoms, and treatments are different.
IBS is a class of functional gastrointestinal disease. It affects how the intestine work, causing them to contract further (or occasionally less) frequently than usual. IBS is also known as a discontinuous colon and nervous abdomen.
IBS doesn’t inflame or damage the bowel like IBD, so imaging reviews can’t determine it and it doesn’t accelerate the threat of colon cancer. People suffering from IBS infrequently need hospitalization or surgery.
IBD shouldn't be confused with irritable bowel cycle or IBS. Although people with IBS may suffer some analogous symptoms to IBD, IBD and IBS are genuinely different. Irritable bowel syndrome isn't caused by inflammation and the tissues of the bowel aren't damaged the way they're in IBD. Treatment is also quite distinguishable.
G. When to see a doctor ?
See your doctor if you a persevering alteration in your bowel habits or if you have any of the signs and symptoms of inflammatory bowel disease. Although inflammatory bowel complication generally is not fatal, it's seriouscomplications that, in some cases, may catalyze life-threatening complications.
H. Which treatment issuited for inflammatory bowel disease ?
A. Treatments for Crohn’s Disease
As many as 7 out of 10 people with Crohn’s disease ultimately require surgery when cures no longer give symptom relief.
During a bowel restriction, a doctor –
1. Removes the infected bowel segment.
2. Connects the two ends of the well-conditioned bowel.
After surgery, the hanging around part of the bowel adapts and functions as it did ahead. Roughly 6 in 10 people who suffer surgery for Crohn’s disease will have a recurrence within 10 times. Another bowel resection might be a good option for the patient.
Treatments for Ulcerative Colitis
With 30+ years of life with ulcerative colitis, 1 out of 3 people need surgery. A Surgeon -
1. Removes the colectomy or the colon and rectum.
2. It connects the anus and small intestine.
3. It helps to create an ilea pouch that accumulates stool, which then exits through the stool.
Not often, you may need an ileostomy rather than an ileal pouch. An ileostomy pouch attaches outside of the stomach to collect stool.
A proctocolectomy is curative. Symptoms won’t replace after surgery to take off the colon and rectum. Still, you may have problems with the ileostomy or ileal poke, similar to pouchitis (inflammation and infection).
I. Which treatment issuited for inflammatory bowel disease ? Ayurveda or Homeopathy
Role of Ayurveda in treating IBD -
Complementary Alternative Medicines (CAM) use the approach of Ayurvedic Medicines which include herbal and plant remedies, oils, and spices, as well as meditation, which may help ease ulcerative colitis symptoms during the times when the situation worsens.
Before you form any melodramatic fluctuations in your diet, consult with your doctor or dietitian to see if some foods may cause distress. An Ayurvedic diet promotes and supports balance and has specific guidelines for each dosha.
When the pitta dosha is out of equilibrium, colon function is blemished. Eggs are one food that's understood to support equalizing the pitta dosha.However, you may retain milk, ghee, If you’re not lactose intolerant. full-fledged fruit is allowed, like apples, pears, pineapples, melons, and mangos.In Ayurvedic rehearsal, acupuncture is used at distinct points on the body that will effect a cure. In the United States, an Ayurvedic practitioner who performs acupuncture must be certified as a traditional Chinese drug practitioner in utmost countries.
Examinations of Ayurvedic acupuncture are scarce. According to the Crohn's & Colitis Foundation, exploration continues to estimate the benefits of acupuncture beyond managing aches. But while some examinations have displayed that acupuncture may improve symptoms, effects vary.
Role of Homeopathy in treating IBD –
Homeopathy can be authentically efficient in dealing with inflammatory bowel disease. This form of treatment not exclusively reduces the intensity of the symptoms being endured but addresses the root cause of the issue and keeps it from duplicating constantly. Homeopathic medications have inconsiderable side effects and can be safely defined for children and grown-ups of all periods. This medicine can be taken alongside other forms of remedy as well. Still, self-medication isn't advised. This is because homeopathy is a form of constitutional medicine where the ideal remedy is grounded on the symptoms shown as well as the patient’s overall physical and intellectual health. Therefore, a remedy that's effective for one person may not be correspondingly effective for another.
While some homeopathic remedies are specified for cases experiencing diarrhea that worsens in the morning, patients who complain of diarrhea that's worsened at night may be prescribed a different medication. medicine is also dependent on the foods that trigger bowel irritation. For illustration, distinguishable homeopathic remedies are demanded patients who complain of diarrhea deteriorating by eating fruits and milk and those who get diarrhea after eating meat. The patient’s life can also impact the remedy. For illustration, some patients may prefer cold water while others prefer to drink warm water. The same medication cannot be prescribed to both of these cases.
J. Here are some things that you need to take care off -
1. Lifestyle Changes
Certain nutritional and life factors can frame IBD symptoms worse. Still, making positive changes to these habits can help a person manipulate their symptoms, reduce flares, and indeed maintain remission.
2. Stress
Some people with IBD experience more severe symptoms during a stressful time.
Some stress management methods are -
1. Exercise
2. Meditation
3. Breathing Exercises
4. Muscle Relaxation
3. Emotional Support
IBD can have a significant and major emotional impact, especially on those with severe symptoms of IBD. For this reason, it’s important to have a strong support network among house and friends. People suffering from IBD should consider joining a support group or going to counseling sessions, which they can find better.
#bestcardiologistinnavimumbai#heartspecialistinnavimumbai#bestheartdiseasetreatmentinnavimumbai#cardiologistinmumbai#besthearthospitalinnavimumbai
0 notes
Photo
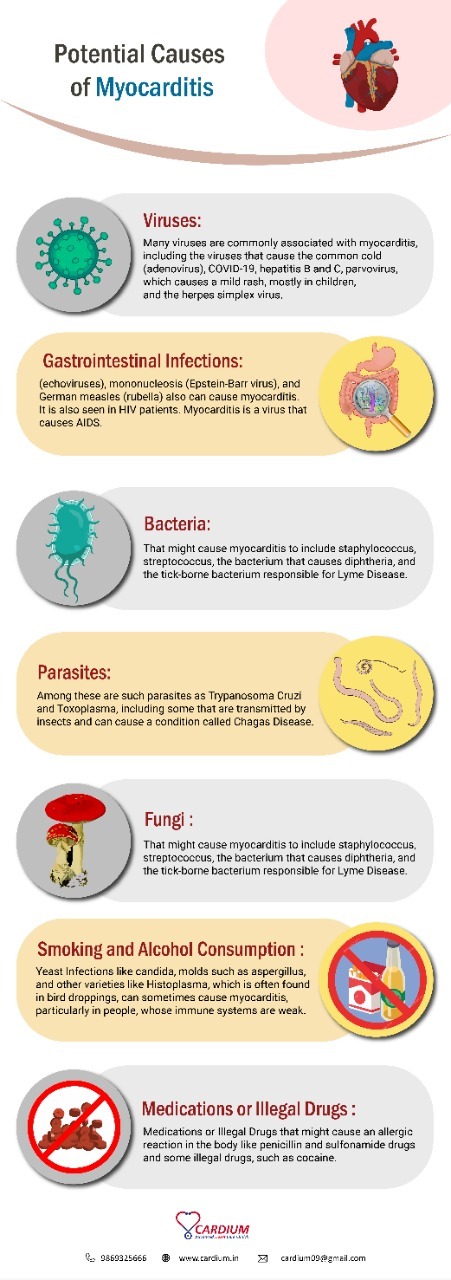
In this Infographic, we have explained to you the different causes of Myocarditis, and all their symptoms. We have given this information in a short and simple way.
#cardiologistinavimumbai#heartspecialistinnavimumbai#bestheartdiseasetreatmentinnavimumbai#besthearthospitalinnavimumbai
0 notes
Text
Some Important Things You Should Know about Myocarditis

What does "myocarditis" mean ?
Myocarditis is a term used to describe the inflammation of the cardiac muscle, known as myocardium. This condition belongs to a group of diseases that affect the heart muscle, known as cardiomyopathy. Cardiomyopathy is referred to as a group of diseases that mainly affects the cardiac muscle (myocardium). In cardiomyopathy, blood flow to the heart muscle is restricted, which makes the heart muscle work harder, to the limit where it enlarges and stiffens, causing the death of the tissues of the muscle. Cardiomyopathy is one of the main causes of a heart attack or heart failure. If left unattended, it can lead to serious consequences like the formation of blood clots in the affected area. This happens when the plague deposits harden and crack, platelets arrive at the affected area that can cause a blood clot in the coronary arteries. This obstructs the blood flow, leading to possible heart failure or sudden cardiac death, for athletes who have cardiomyopathy if neglected, can even lead to sudden cardiac death.
What causes acute myocarditis ?
Potential causes of myocarditis include :
1. Viruses - Many viruses are commonly associated with myocarditis, including the viruses that cause the common cold (adenovirus), COVID-19, hepatitis B and C, parvovirus, which causes a mild rash, mostly in children, and the herpes simplex virus.
2. Gastrointestinal infections - (echoviruses), mononucleosis (Epstein-Barr virus), and German measles (rubella) also can cause myocarditis. It is also seen in HIV patients. Myocarditis is a virus that causes AIDS.
3. Bacteria - that might cause myocarditis include staphylococcus, streptococcus, the bacterium that causes diphtheria, and the tick-borne bacterium responsible for Lyme disease.
4. Parasites - Among these are such parasites as Trypanosoma cruzi and Toxoplasma, including some that are transmitted by insects and can cause a condition called Chagas disease.
5. Fungi - Yeast infections like candida, molds such as aspergillus, and other varieties like Histoplasma, which is often found in bird droppings, can sometimes cause myocarditis, particularly in people, whose immune systems are weak.
6. Smoking and alcohol consumption - actively smoking or consuming alcohol makes the blood sticky, and it is most likely to clot, which can obstruct the blood flow to the heart. It also lowers good cholesterol in the body.
7. Medications or illegal drugs that might cause an allergic reaction in the body like penicillin and sulfonamide drugs and some illegal drugs, such as cocaine.
What is Viral Myocarditis ?
Viral myocarditis has been recognized as a cause of congestive heart failure for people who are over 50 years. This disease is still difficult to treat. Even with a proper diagnosis, there are still no medical treatments to prevent the development of subsequent dilated cardiomyopathy (DCM) and in this case, death can occur at some point. Inflammation of the heart muscle, if caused due to viruses like adenovirus COVID-19, parvovirus, and herpes simplex virus, then it is known as Viral myocarditis. This disease, if not cured on time, can lead to adverse cardiac muscle complications like a type of cardiomyopathy where the heart enlarges and is not able to pump blood properly, known as Dilated Cardiomyopathy. It mainly includes enlargement of the ventricular cardiac muscle, the main causes being the use of cocaine, consumption of alcohol, the influence of genetics, complications during pregnancy, and infections. Symptoms include swelling of legs, chest pain, fluid build-up in lungs, etc. The virus, if it enters the body, either attacks the cardiac muscles or the immune system. The inflammation in response to that viral infection leads to damage in the cardiac muscle. The severity of myocarditis depends on each patient. The toxins secreted by the virus causes damage to the muscle cells(also known as pacemaker cells) of the heart. The duration of this infection is about three days. The defense mechanism although slows the procedure of viral replication, replication of this virus is sufficient enough to cause severe cardiac decompensation at a rapid rate. The factors that affect this damage are age, exercise, and nutrition. These are the main factors but at the same time pregnancy and sex hormone status play a role in the development of myocarditis. If the immune system fails to control the beginning of the viral replication process, it may lead to cardiomyopathy.
Is myocarditis permanent ?
Myocarditis can interfere with the normal functioning of the heart, and the cardiac muscle can be permanently damaged. Scar tissue may form due to the inflammation of the myocardium and might increase the risk for abnormal heart rhythms (Arrhythmia). But myocarditis can be cured by:-
1. Medications - medicines like Enalapril are given to reduce blood pressure or Warfarin is given to prevent blood from clotting, The medications include SGLT2 inhibitors or gliflozins which reduce blood glucose levels without activating the release of insulin from the pancreas. They also reduce blood pressure in diabetic patients. Medications like SGLT2 inhibitors and GLP-1 help reduce obesity, hypertension, and blood sugar levels since these three factors contribute to heart diseases. PCSK9 inhibitors are also given to reduce cholesterol levels or low-density lipoprotein in the patient's circulatory system.
2. Therapies and surgeries - Therapies like alcohol septal ablation procedures involve injecting alcohol(ethanol) into the part where the heart muscle has thickened. It kills the cells of the muscle shrinks the diseased tissue and restores blood flow to the heart muscle. Surgeries like implanting a ventricular assist device are used to pump blood in the body when the patient has gone through myocardial infarction or if the patient is suffering through heart failure.
3. Installation of an Artificial Pacemaker - this device generates electric impulses by the electrodes present in the device that makes the lower and upper heart chambers contract to pump blood. This device regulates the normal function of the electrical system of the heart. Its main purpose is to restore the normal rate of the heart which was either very slow or very fast earlier due to a defect in the natural pacemaker of the heart.
4. Intra-aortic balloon pump - used in percutaneous coronary angioplasty. It is done by placing a catheter through the blood vessel into the heart. The balloon is placed at the tip of the catheter. When it is blown, it forces the valve to open. The balloon valvuloplasty is done in mitral, aortic, or pulmonary valves.
5. Heart valve replacement - Surgical Aortic Valve Replacement, where the stiff aortic valve is replaced through an open-heart surgery procedure, where the sternum is opened and a heart-lung machine is used to continue pumping of blood in the body while the heart is stopped for the removal of the valve. Transcatheter Aortic Valve Replacement, on the other hand, is for those who cannot physically go through surgery and cannot take blood thinners, transcatheter aortic valve replacement is the only treatment. Even for such patients, TAVI is the safest method for replacing the damaged valve, where access to the heart is gained by inserting a catheter through an accessible blood vessel.
Q. What viral infection causes myocarditis ?
The viral infections that are responsible for myocarditis are :-
1. common cold (adenovirus)
2. Coxsackie B viruses
3. Epstein-Barr virus
4. Cytomegalovirus
5. Hepatitis C
6. Herpes
7. HIV(AIDS)
8. Parvovirus
9. Chlamydia (a common sexually transmitted disease)
10. Mycoplasma (bacteria that causes lung infection)
11. Streptococcal bacteria
12. Staphylococcal bacteria
13. Treponema (the cause of syphilis)
14. Borrelia (the cause of Lyme disease)
15. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2)
The virus, if it enters the body, either attacks the cardiac muscles or the immune system. The inflammation in response to that viral infection leads to damage in the cardiac muscle. The severity of myocarditis depends on each patient. The toxins secreted by the virus causes damage to the muscle cells(also known as pacemaker cells) of the heart. The duration of this infection is about three days. The defense mechanism although slows the procedure of viral replication, replication of this virus is sufficient enough to cause severe cardiac decompensation at a rapid rate. The factors that affect this damage are age, exercise, and nutrition. Although other factors such as pregnancy and status of sex hormone play their role in the development of myocarditis. If the immune system fails to control the beginning of the viral replication process, it may lead to cardiomyopathy.
Why is exercise bad for someone with myocarditis ?
One of the complications of myocarditis is the possible development of an abnormal heart rhythm or Arrhythmia, that can hamper the overall cardiac health of the individual. Arrhythmia is a condition referring to abnormalities in heartbeats due to issues in the electrical conduction system of the heart. When the heart beats too slow, it is known as bradycardia, and when beats too fast, it is known as tachycardia. In some cases, arrhythmia arises with no symptoms. Symptoms, if present, may include shortness of breath, palpitations, chest pain, sensing a pause between heartbeats, blackouts, etc. In a few situations, it may even lead to heart failure or sudden cardiac death. If you exercise when you have myocarditis, the risks of developing an abnormal heart rhythm become significantly higher, and serious abnormalities can occur like:-
1. Cardiac arrest - Arrhythmia cause an increase in the formation of blood clots. Blood clots can obstruct the blood flow to the heart, which can cause cardiac arrest due to loss of blood flow throughout the body.
2. Stroke - A blood clot, if it breaks loose from the coronary arteries, can also travel to the brain, causing a stroke.
3. Heart failure - Arrhythmia can cause the failure of the heart to pump blood efficiently.
#bestcardiologistinnavimumbai#cardiologistinnavimumbai#besthearthospitalinnavimumbai#heartspecialistinnavimumbai#bestheartdiseasetreatmentinnavimumbai
0 notes
Photo
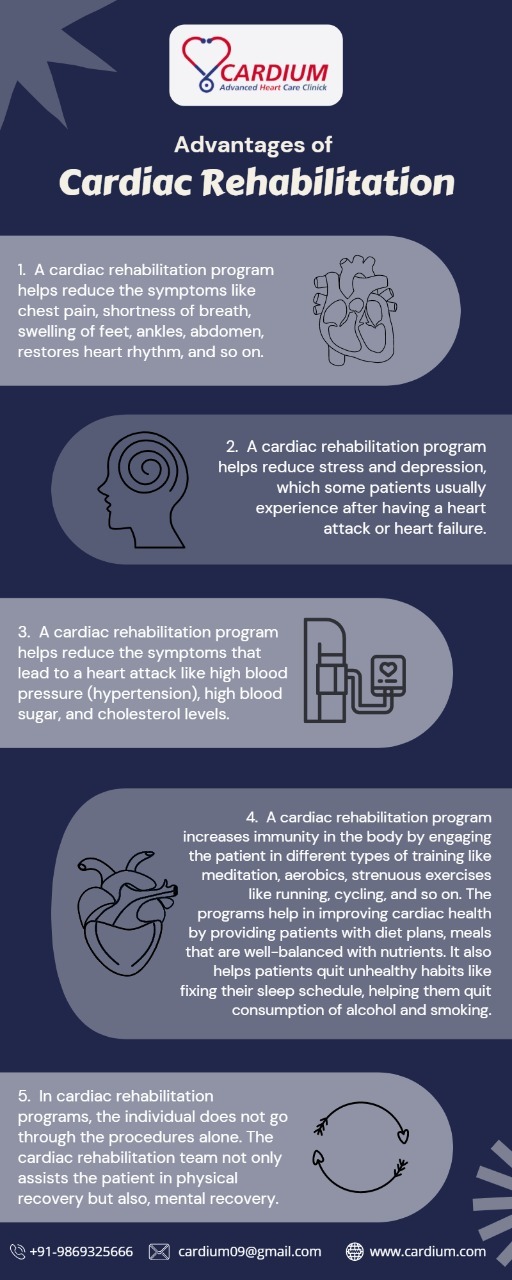
In this Infographic, we have explained to you the benefits of cardiac rehabilitation program. Here's a look at some of the heart diseases that cardiac rehabilitation protects you from, as well as what types of exercises are done in this program and how it benefits your body.
#bestcardiologistinnavimumbai#besthearthospitalinnavimumbai#heartspecialistinnavimumbai#cardiologistinnavimumbai#bestheartdiseasetreatmentinnavimumbai
0 notes
Text
Cardiac Rehabilitation and It's Importance

What is Cardiac Rehabilitation, and How is it important ?
Cardiac Rehabilitation programs are medically supervised programs to assist those patients who have gone through heart diseases like coronary artery disease, myocardial infarction, peripheral artery disease, heart failure, arrhythmia, people who have gone through heart intervention programs like surgical aortic valve replacement, transcatheteraortic valve replacement, angioplasty, etc. The cardiac rehabilitation program's main motive is to provide support to cardiac patients to reduce the physiological and psychological distress that accompanies such heart ailment accidents. Their goal is to reduce any second incident of cardiovascular disease, improve the heart's functioning capacity, and increase the patient's confidence.
After going through an episode of a heart attack or any cardiovascular disease, it is not easy to get your life back on track. It becomes difficult for the concerned individual to track their health properly because :-
While engaging in vigorous training, you might not be able to identify pain that might affect your health if not treated on time.
The basic wellness program that you might have chosen might not cater to your needs. This might make you lose interest in engaging in any programs of this kind.
Without a properly scheduled exercise regime, you might lose track as to when and how the training should be done. There can be a possibility that the individual is not following the schedule and is resuming their previous unhealthy habits. Without digital health tracking, wellness programs lack discipline.
The individual might be unaware that they are following an improper diet. This might cause further cardiac complications.
Therefore, an individual needs to enroll in a cardiac rehabilitation program so that they can systematically monitor their health.
What are the Advantages of Cardiac Rehabilitation ?
The advantages of enrolling oneself into a cardiac rehabilitation program are :-
1. A cardiac rehabilitation program helps reduce the symptoms like chest pain, shortness of breath, swelling of feet, ankles, abdomen, restores heart rhythm, and so on.
2. A cardiac rehabilitation program helps reduce stress and depression, which some patients usually experience after having a heart attack or heart failure.
3. A cardiac rehabilitation program helps reduce the symptoms that lead to a heart attack like high blood pressure (hypertension), high blood sugar, and cholesterol levels.
4. A cardiac rehabilitation program increases immunity in the body by engaging the patient in different types of training like meditation, aerobics, strenuous exercises like running, cycling, and so on. The programs help in improving cardiac health by providing patients with diet plans, meals that are well-balanced with nutrients. It also helps patients quit unhealthy habits like fixing their sleep schedule, helping them quit consumption of alcohol and smoking.
5. In cardiac rehabilitation programs, the individual does not go through the procedures alone. The cardiac rehabilitation team not only assists the patient in physical recovery but also, mental recovery.
How is cardiac rehabilitation used to treat heart failure ?
Even though heart failure is a serious condition and if not acted on time can worsen with time, there are various treatments and recovery plans that prevent the risk of stroke or if the individual has had a heart attack, it prevents the second episode of it. One of the most effective treatment plans in which cardiac patients can enroll is a cardiac rehabilitation program. The main purpose of a rehabilitation program is to help people live longer by improving the symptoms that increase the risk of heart ailments. It also depends on the patient's condition.
A cardiac rehabilitation program aims in maintaining cardiac health by engaging the patients in exercises like cycling, brisk walking, aerobics, Zumba, and other forms of training. Cardiac rehabilitation programs also provide patients with diet plans, weight-reducing instructions, meals that are balanced with nutrients like vitamins, minerals, proteins, roughage, and so on. This is essential for those patients whose hearts have failed to function properly, as sticking to a fitness regime may improve their cardiac functioning.
Cardiac rehabs educate and counsel their patients so that they are aware of their sessions, training, diet plans, etc. The patients must be mindful of the seriousness of their condition and are taking effective steps for their speedy recovery. This makes the patients aware that they must take effective steps for recovery.
Cardiac rehabs make sure that their patients are taking the medicines that they have been prescribed. Sometimes, especially older patients who have congestive heart failure, forget to take their medicines. The cardiac rehabs, with the help of the cardiac rehabilitation medicine tracklist, regularly monitor whether their patients have taken the medicines as scheduled.
In many cases, heart failure patients lose the desire to recover. They spent days repenting about how things went wrong and evaluating their past. In some situations, heart failure patients also suffer from post-traumatic stress disorder, depression, and other mental issues. So the cardiac rehabilitation team encourages their patients and keeps them in a positive environment to instill hope and belief that they are not alone, and they will recover soon.
What are the benefits of a cardiac rehab program after having cardiac bypass surgery ?
Cardiac bypass surgery is done to restore blood flow to the dying cardiac muscle. The procedure is carried out by making an incision on the chest cavity for the surgeon to get access to the coronary artery which is blocked. Then the cardiac surgeon will find an artery from your chest wall (an internal mammary artery) and attach it to the blocked coronary artery, with the help of sutures. Even though bypass surgeries help in treating blocked arteries, it takes a long time for a patient to recover from coronary bypass surgery. After any type of surgery, it takes a long time for the patient's body to regain muscle strength. So, cardiac rehabilitation programs, help their patients in regaining cardiac strength by :-
Consulting various treatment plans that cater to their conditions. The patient must be aware of all types of treatment plans and their consequences and risks. So, the specialists curate a list of treatment plans according to the patient's condition and let them choose.
After the patient has decided on its preferable treatment plan, the cardiac rehabilitation team, which mainly comprises exercise physiologists, cardiac imaging specialists, nurses, physical therapists, nutritionists, preventive cardiologists, psychologists, and therapists, works together to provide necessary services to their patient.
The cardiac nurses provide a cardiac rehabilitation medicine tracker to the patients so that they remember when to take their medicines.
The exercise physiologists engage the patients in regular physical training like walking, meditation. They avoid exercises like running, weightlifting, shoulder and arm exercises, etc.
The nutritionists provide a strict diet plan to the patients that include daily consumption of a measured quantity of vegetables, fruits, whole grains like oats, muesli, and nuts. The patients should make sure that they consume less amount of sugar, table salt, red meat, and all types of processed foods.
Mental health professionals like psychologists and therapists speak to those patients that are suffering from mental distress like anxiety, trauma, and depression. They will assure their patients that they are in a safe space, and they will recover soon.
What are the 4 Phases of Cardiac Rehabilitation ?
The Four Phases of Cardiac Rehabilitation Programs are:-
1. The Acute Phase - This phase starts right after the patient physically recovers to some extent after cardiac surgery. A physical therapist of the particular medical facility will be recommended to the individual by the faculty's senior cardiologist so that the individual's body returns to its normal functioning. The physical therapist will explain all about the cardiac rehabilitation program to the patient and their family members so that they all are aware of the program's procedure, risks, and consequences. After you are discharged from the medical facility, you will be enrolled in the program, where phase two starts.
2. The Subacute Phase - This phase starts right after the patient leaves the medical facility and enrolls in a cardiac rehabilitation program. This involves a cardiac rehabilitation team involving an exercise physiologist who will monitor the heart's response to cardiac exercises. Nurses, pathologists, and physical therapists will do a few tests like blood pressure tests, checking height, weight, cholesterol level to see whether the patient is still suffering from any risk factors like hypertension or diabetes. Then cardiac imaging specialists and nurses will do a few scans like ultrasound, CT scan (computed tomography), MRI scan, electrocardiogram, and echocardiogram to check the heart's electrical conduction system. Depending on the tests and scans, the physical therapist will educate and prescribe exercises, diet plans, and medicines accordingly.
3. Intensive Outpatient Therapy - After the patient has been educated about its exercises and diet plans, the patient is then monitored without any supervision. This is done to check the patient's knowledge about the types of exercises it has to do, the kind of diet it has to take, the time at which medicines need to be taken, and so on. If the patient performs these tasks correctly, then they are discharged from the rehab.
4. Independent Outpatient Conditioning - This is the last phase where the patient carries out the treatment program independently since by now, the patient has developed a clear understanding of their treatment plan. All the activities of the patient are monitored by the physical therapist.
#cardiologistinnavimumbai#cardiologistinmumbai#bestcardiologistinmumbai#heartspecialistinnavimumbai#taviinmumbai#heartcareclinic#heartcaretreatmentinnavimumbai
0 notes
Photo
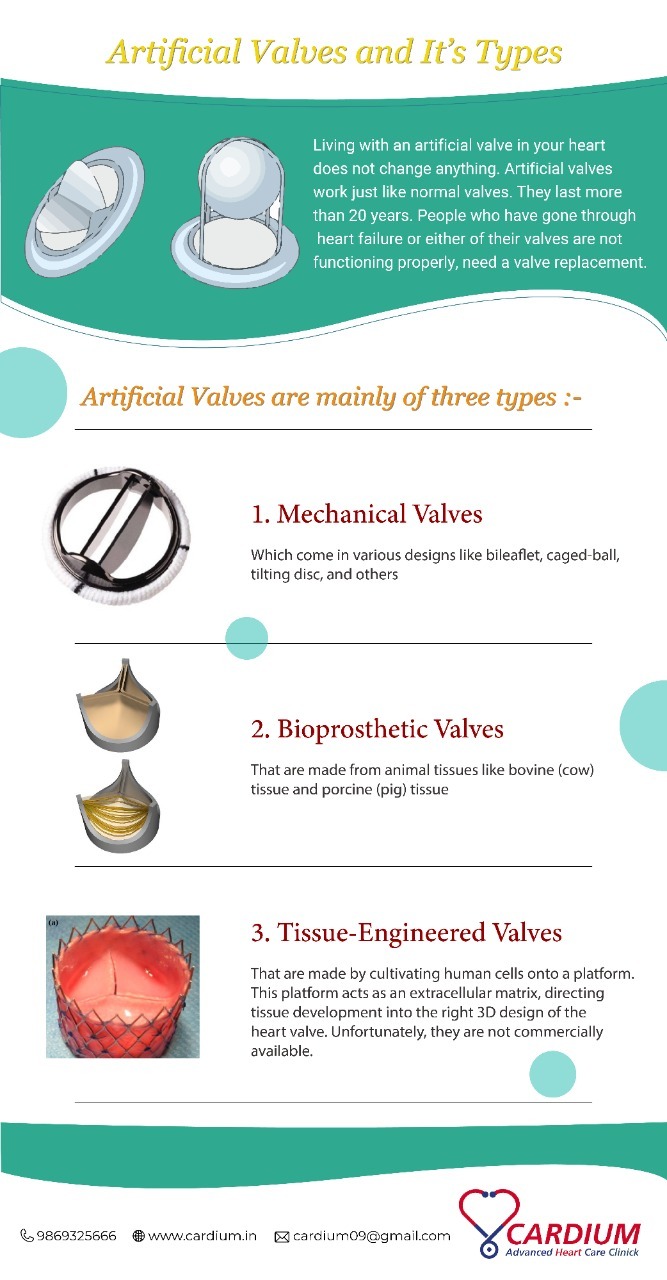
In this Infographic, we have briefly explained to you, what an artificial valve is, why do you need it and what its types are.
#cardiologistinnavimumbai#cardiologistinmumbai#besthearthospitalinmumbai#besthearttreatmentinnavimumbai#bestheartdiseasetreatmentinnavimumbai#heartspecialistinnavimumbai
0 notes