#neuropsychology
Text
when the neuropsychologist running tests on me tells me, a painter, that my visual processing centers are very developed

127 notes
·
View notes
Text
the prefrontal cortex is the site of decision-making, thought and emotional regulation. it develops until the age of 25 years.
which means,
you don't have to beat up yourself for things you did before you turned 25 that were not your proudest moments. yes, we mess up. yes, it has consequences. but your brain quite literally was incapable of making the most perfect adult decisions all the time by that age.
even people older than that can have a lapse of judgment. so, it is absolutely normal if you do/did as well.
as long as you learn and grow from your mistakes- it is okay. you are/were a really young person. we are all doing it for the first time.
#also it is fucked up to think 18 year olds should have their lives figured out right after high school#they're just children#allow them to explore and make mistakes#mental health#mental health awareness#mental health support#mental health reminders#coping#positivity#reminders#wellness#kindness#therapy#psychology#neuropsychology#the brain
141 notes
·
View notes
Text
The Myth of Dreamless Sleep
Consciousness never "switches off" because it isn't generated by the brain. Its sensory inputs can be switched off - during sleep or general anesthesia, for instance - but your consciousness is still there. For example, a small but consistent number of patients report out-of-body experiences (OOBEs) or near-death experiences (NDEs) while under general anesthesia.
#consciousness#dreams#out of body experience#near death experiences#nde#oobe#cognitive neuroscience#neuropsychology#neurology#sleep#rem sleep
29 notes
·
View notes
Text
Extremely Scientific™ Diagram of the Neurophysiology of Executive Dysfunction

40 notes
·
View notes
Text
It's uquiz time baby! For context Clara's our psych teacher and we hate her x
34 notes
·
View notes
Text
Happy Halloween Half-Way!!!
Doc Heath here; your friendly Neighborhood NeuroMechanic!
Spooky season is a great time for the young AND the young at heart to PRACTICE “FEAR”. That’s right! Practicing experiencing difficult emotions when we know we’re in a safe environment can help us program our minds to understand emotions - even the difficult ones - are not harmful to us.
Go ahead and enter the creaky doors of that Haunted House. Watch that spooky movie and let the CHILLS run up and down your spine. Decorate your home and yard with ghosts and monsters and witches and zombies; later imagining them all coming to life in the dark of the night.
Guess what will happen when you experience that FEAR? N-O-T-H-I-N-G.
Fear can never harm you though it can be a difficult emotion.
Use this Half-Way to Halloween to create a space for fear that YOU control.
Feel the fear and THEN pay attention to your THINKING. After all, it is your THINKING that is CREATING the fear in the first place.
Change your thinking; change your feelings. Master your thinking; master your life.
TherapyBites Podcast NOW AVAILABLE on your favorite pod player!
It’s all about the Psychology of EveryDay Life & Relationships.
SIX BRAND NEW episodes:
E1. Bonus Intro Episode
E2. Scary Stories from the DARK RECESSES Beneath the Therapy Couch
E3. Spooky Tales, Scary Therapy, & Staying Psychologically Safe
E4. Barking Werewolf Ruins the Day
E5. Zombies & Depression Quicksand
E6. Spirits, Unsafe Spaces, & Other Tales of Terror
E7. Myths, Monsters, & Scary Stress
#therapybites#couchcrumbs#psychotherapy#relationships#neuroscience#docheath#bitesizedtherapy#cognitive science#neuropsychology#forensic psychology#podcast#therapistsoftiktok#therapistsofinstagram#best therapy#therapytok#therapymemes#marriagecoach#christian marriage#marriage counseling#success coach#success#mindsetcoach#halloween#spooktacular#spooky#scarey#get scared#frightfest#fright#zombie
322 notes
·
View notes
Text

Anna Maria Island Florida :: (Florida beaches USA)
* * * *
"Here are 6 ways to regulate yourself using neuropsychology:
If you are stressed, use the physiological sigh. Huberman lab talks about it, but it’s essentially two inhales and one long exhale, and you do that over and over again.
If you are anxious, go for a walk. It deactivates your amygdala.
If you are sad, acknowledge your feelings and then move your body. it release endorphins.
If you are impulsive, like angry. You can’t think straight. Look out the window and don’t look at anything. Just like dilate your gaze. It blunts your neuroadrenaline so you can think clearly.
If you have low motivation, this is interesting ~ focus on one spot on your screen for one minute. Ignore everything else. Pupilary convergence increases focus.
And finally, if you’re feeling insecure, low self-worth, write down your strengths. Logical thinking overrides your limbic system."
~ Ana Del Castillo / Women's Rightness & Empowerment Expert
[alive on all channels]
#disregulation#regulation#Ana Del Castillo#women's rightness & empowerment#Anna Maria Island#Florida beaches#the sea#advice#neuropsychology
16 notes
·
View notes
Text
If a community disability term, such as neurodivergence, contains diagnoses that in your experience are too different to be related, you can opt out of the term, but you do not get to disagree that the term still includes both for other people with those diagnoses.
I don't actually care what the coiner's intentions with a word were that much, beyond, "if even one person finds a wider or more inclusive definition meaningful, the definition expands to encompass their usage of it".
That's descriptivism, the idea that words only exist to be useful to us and that we shape their meaning to that end. It is the counterpart to prescriptivism, the idea that words have concrete, strict, static definitions and that we have to use the right words as accurately as possible and can't use words if they fit badly enough.
"Words have meanings" is a prescriptivist take, but so is "I don't feel neurodivergence includes xyz".
I mean this in a way less aggressive than it sounds, but quite simply, neurodivergence doesn't revolve around your experience of it.
I also find it symptomatic of the extreme cartesian dualist bias most people haven't actually examined that "physical disability" can include everything from neurogenic pain to irritable bowel disease to limb deformities to cardiac issues to asthma to paralysis to visual impairment and more, but neurodivergence and neurodisabilities are often limited to, if not the more palatable and less disordered forms, even just things that are primarily cognitive or emotional in nature.
To explain, cartesian dualism is the idea that there is a separate, nonphysical "mind" from the physical neurological structure of your brain and body - and that therefore essentially mental illness and neurodivergence are sicknesses and differences of an abstract consciousness that is little more than a different word for the idea of a "soul".
It's very disturbing to me that people think that, because we don't fully understand how bioelectrical and chemical processes or neurophysical structure inform the phenotypical presentation of disorders and neurodivergence with an array of cognitive-emotional symptoms, that we can simply just say "eh, it's not physical in the same way physical neurological symptoms are.
Okay, that's a mouthful, but basically, our entire consciousness - emotions, thoughts, the places in our physical bodies we feel our emotions (and store trauma), the physical symptoms of our mental illnesses, and so forth - they all are caused by one of essentially three categories of things.
Either the electrical signals passing between neurons in a certain order and direction, hormones and enzymes and proteins being chemically processed by receptors in brain and other bodily cells (which, it's important to note, mental illness and neurodivergence exist as a conversation between brain cells and other bodily cells), or the actual physical shape of the brain.
From what little we do understand, we know that electrical activity, chemical activity, and physical differences in the brain are responsible in some way for the psychological phenomena we study. We mostly just don't understand exactly HOW.
The similarities between primarily physical neurological conditions and primarily mental neurological conditions is that they are both a result of what is occurring in the neurological system (and to a lesser extent, in where the neurological system interfaces and communicates with other systems).
Migraines, nerve pain, epilepsy, bell's palsy, Parkinson's, tremors, stroke, lateral sclerosis - these are very different from things like bipolar, anxiety, OCD, NPD, AvPD, SzPD, PTSD, DID, autism, schizophrenia, ID, and so on, for many people.
It's why you can opt out of labels like neurodivergence for conditions you don't feel it fits.
But, crucially, you don't get to make that decision and universally define the word for others. The most inclusive definition of the word prevails, because there are people who do find that their experiences with things in each of those category are similar, or so closely related they can't be separated, or simply worth grouping together for the fact they occur in the same bodily system via the same or similar mechanisms.
For me, my chronic pain, my gut health issues, my MCAS, my autism, my anxiety, my PTSD, my DID, my chronic fatigue, my brain fog, my schizophrenia, my ADHD, my tremor, my dysautonomia, my balance issues and struggles with spacial awareness and lack of awareness of my physical body, the alexithymia that I've worked so hard to manage, my language and sensory processing disorders... it's all closely and heavily interrelated.
Some of it causes or worsens other parts (or in some cases is minimally suspected to, but I'm mainly focusing on the ones that inarguably directly cause the others here). My anxiety and PTSD trigger my gut issues. Inflammation from my MCAS triggers my chronic pain and brain fog and POTS and makes my anxiety, depression, and DID worse. My dyspraxia and sensory processing are worse when I'm brain foggy or in pain. Getting excited about special interests can make my tremor worse than anxiety can. This is kind of a weird one, but self-injury from BPD has caused nerve damage. Autism and ADHD cause a large portion of my chronic fatigue.
That's without even getting into where the symptom sets overlap.
Anxiety comes with tachycardia, shortness of breath, feelings of dread/doom, stomach upset, tremors, dysregulation of my sense of temperature, flushing, and more.
POTS comes with... tachycardia, shortness of breath, stomach upset, tremors, dysregulation of my sense of temperature, flushing, and more. And MCAS covers the "feelings of dread/doom", so when they are flaring up together...
Chronic pain is a symptom of depression and PTSD as well as fibromyalgia and nerve damage. Chronic fatigue is a symptom of just about every disability that exists.
Food sensitivities are as likely to be from neurodivergence as from eating disorders (which can be considered neurodivergent) as from GI issues. I see an allergist for my condition which is caused by dysregulation of gastrointestinal cells, which is suspected to potentially be related to trauma, which is also suspected as having a relationship with the dysautonomia present in my POTS, trauma for me which is as much a result of my neurodivergence and the casual ignorant and often nonmalicious ableism ingrained into every facet of society I faced as the abuse I went through. (And some of the abuse was a result of my disabilities, both primarily physical and primarily mental!)
There is no separating it for me. They are not different enough to deny myself a label that acknowledges that and never will be. Neurodivergence and neurodisability (a term I coined) as well are as much for people like me as people who have fully discrete separate symptoms.
I even find the separation of disabilities into "physical" and "psychological" to be a bit of a misdirection. Psychological disabilities are physical. They manifest through physical symptoms. Even emotional symptoms are experienced by the body on a physical level, though a lot of us neurodivergent folks struggle with awareness of that (I know I did and often still do).
Anxiety is often a rapid heart rate and sweating and shortness of breath. Depression is pain and appetite suppression and often low blood pressure. Sadness can be chest pain and throat tightness. Excitement often has near identical physical manifestations as anxiety. Happiness is usually felt throughout the whole body. Sensations of different temperatures, breathing, pulse, and gut functions are most primarily associated with emotion.
"Trust your gut" even means "trust your intuition", meaning your subconscious mental sense of safety vs danger, for this reason.
"My heart plummeted."
"My heart was in my throat."
"My stomach was roiling with nerves."
"I felt a cold sweat on my neck."
"I knew in my gut I could trust her."
These are how people describe emotions.
Even where the symptoms are either not identifiably physical or not experienced as physical in the consciousness (such as thought patterns), they are caused by physical processes in an actual physical organ. Their cause is the same at a fundamental level as a primarily physical symptom such as pain - while they may occur in different locations in the neurological system, or may be triggered by different sets of chemicals, at a basic level they are both physically occurring in the same bodily system.
Even separating out the brain as an organ from the rest of the body has actively limited scientific progress. It's only as modern science has actually been analyzing it in concert with the other bodily systems that it is responsible for both controlling and processing feedback from that large advancements in our understanding of neurology have been made.
The organ responsible for telling every other organ what to do and understanding what happens in every other organ cannot be compartmentalized and analyzed on its own. At least, not if we want any actual useful data.
I often wonder, for people who do have discrete symptom sets, is there a reason other than simply "it doesn't make sense to group it with my other neurodivergence" for saying they "disagree" with the definitions of neurodivergence and neurodisability that they are allowed not to use for themselves?
Is it possibly that neuroableism is so rampant in our society and even in disabled spaces that they simply haven't examined their own internalized biases and bigotry and they don't take neurodisabilities, including their own, as seriously as disabilities they consider more physical?
Is the idea that they have been as physical as their other disabilities all along scary or threatening because it means that in shoving them off into the realm of "mental" disability they've been pushing themselves past their limits to "overcome" something that is just as painful, just as harmful, and just as concretely, profoundly disabling as their other disabilities? That they were just as unable to do the things their disability prevented them from doing and hurting themselves just as much by trying to and then blaming themselves on top of it for the ways they "fell short" due to said disability?
This is not meant as an attack. I sometimes have the people who say this stuff unintentionally stumble on trauma triggers, but I don't dislike them. I wish I was more capable of having these conversations without really essentially running and hiding. I try to use this blog for that because I'm able to ignore it more easily than my main blog when I'm in a heightened state, and because it's more of a controlled environment where these conversations are intended to take place.
These are questions I'm asking specifically from analyzing past attitudes of mine. I didn't necessarily share them publicly, but there was a time where I felt similarly. I'm not asking out of some concern-trolling, either. I acknowledge that what I talked about is only one possible explanation for that belief, and if that is the case, I'd simply encourage the people for whom it's true to be patient with themselves and let themselves be disabled, whatever that means for them.
I don't even think it's necessarily a super harmful belief, although I think it crosses a line when the belief goes from "that's not how I use neurodivergent for myself" to "I don't think it's useful for neurodivergence to be defined that way in general". I think it's one we should all interrogate, sure. Providing a possible explanation is my way of trying to open up a conversation about that. Eliminating a possibility as wrong still gets us closer to a more accurate understanding, even at an individual level.
I think put quite simply though, if that is the case, I don't feel condescending and patronizing pity. I'm angry on all of our behalf that we live in a society that so deeply ingrains those ideas into us in order to uphold the oppression of all disabled people, and especially to sow disunity between us to disrupt our efforts at organization and liberation. I'm angry that we've been taught to hurt ourselves in this way. I'm furious that we've been convinced that this is the right way of understanding and dealing with disability.
So, to loop back around and neatly tie this post off with my original point: I would like to motivate people to examine WHY they label certain diagnoses as neurodivergent/neurodisabilities and others as not. I would encourage them to remember that an umbrella label including diagnoses of theirs that they don't want to use that label for doesn't make the definition wrong. I'd remind them that they are absolutely welcome to use a more restrictive definition individually without challenging the general definition, because words can mean multiple things.
And I'd say that the most important thing is just to remember when discussing this is that other people may consider a shared diagnosis to be neurodivergent where you don't, and that "disagreeing" with them is fundamentally "disagreeing" with their identity and how they experience it, which however well-intentioned is still bigotry. It doesn't make you a bad person, but it is a harmful action and the right thing to do is whatever needs to be done to not continue to harm others. Whether it's as simple as just stopping or as complex as analyzing the entire lens through which you view neurodivergence, the important thing is respecting that neurodivergent identity means different things for different people.
And after all, at least in English, 95 percent of the 3000 most frequently used words have multiple meanings, as do 100 percent of the top 1000 most used words. Words like go and set have upwards of 300-400 definitions! Rather than treating definitions like a math problem, right or wrong, let's treat them as interpretive, and facilitate communication by asking people which they mean.
#prescriptivism#descriptivism#mod stars#unitypunk#neurodivergence#neurodisability#disability#physical disability#neurology#neuropsychology#cartesian dualism#cw brief self harm mention#ableism#neuroableism#trauma#adding this in the tags: a good example is how lqbtqia+ people can opt out the reclaimed label queer#whether your identity is always considered valid as a queer identity or faces bigotry at every turn you can choose to demand inclusion#no matter whether or not you use the label queer#that's important
16 notes
·
View notes
Text
Psychology academics are not here to treat you with kid gloves, sweetness and love and tell you what you want to hear
I work in film. I'd already gotten a uni degree, I was happy, and then I got into reading psychology books and became hooked. And when I became hooked, I got myself a BSc in Psychology out of pure fascination for the subject.
I am not a therapist, nor a counsellor, purely because I still work in film, I love working in film, and psychology is a passion which I find extremely helpful in my work and in my life, but I have no desire to spend every day of my life listening to people's drama. Sounds cold? Well, welcome to science.
But obviously in social media one finds all kinds of things, and I'm always interested in anything related to psychology, so one thing I keep finding is people, somehow, always assume if you know psychology you must constantly treat people like they're injured animals and you're a vet? We must be sweet and loving with complete strangers, and treat them with kid gloves, as if the air might hurt them??? It's wacky.
Anybody who knows anything about psychology knows you ought to distance yourself emotionally from mentally sick people, or else it'll kill you. You've got to be a scientist, be objective, not get attached, not get emotionally involved. And it isn't our duty to treat people like they're fragile. Our duty is to be honest, to do what we can to help out, specially for those who are actual therapists, and only when paid to do so, because hey, it's a job.
Psychology isn't there to pamper people, make them feel better and tell them what they want to hear. Psychologists who do that are the shit ones who then cause a ton of trouble. Psychology is a science, it looks at things objectively, and if you're a piece of shit, it's supposed to hold you accountable, to make you responsible for your actions and to help you have the right tools to turn your life around. But responsibility and accountability are essential in any self-respected therapy, so don't expect to be pitied and given a hug if what you need is a bloody wake up call.
#psychology#science#brain#medicine#mental health#social sciences#lgbtq+#mental problems#neuropsychology#eugenics#sciece
9 notes
·
View notes
Text
Please google the definition of synesthesia before voting if you don’t know what it is! /pos
I’m beginning my thesis research on autism and synesthesia and how these are processed in the same part of our brain and can affect each other!! Not a deeply researched part of psychology/neuropsychology but something i’m super excited to dig into! (This isn’t really something I can include in my research due to having no evidence to back up voter profiles, I’m just interested to see!)
Let me know as well what other co-occurring symptoms you have or one thing you’ve always wondered is connected to autism!! :-)
(For all my autistic friends, I am autistic and conducting this research, so I promise to do so in the best possible way for us!!)
36 notes
·
View notes
Text
The Bipolar Brain: An Introduction
Key Terms
Bipolar: Previously called 'manic-depression' due to the nature of the mania being rooted in depression, this mood disorder is characterized by periods of mood shifts between a manic and depressed state.
Depression: A period of rest after deeply distressing events
Dopamine: A brain chemical meant to encourage pleasure, satisfaction, and motivation.
Grey matter: Also known as the cortex of the brain, this is the outer layer of the brain allows a person to have control over movement, memory, and emotions by sending signals between the different parts of the brain.
Hippocampus: The part of the brain where memories are "stored" to later be relayed to other parts of the brain, consciously or not. It is one of the deepest parts of the brain structure, making signals difficult to send or receive.
*Hypomania: A form of mania that is less severe or impactful than true mania.
Limbic system: Processes emotions and behaviors to help other parts of the brain understand survival necessities.
*Mania: A false sense of euphoria, triggered by stress
Prefrontal Cortex: The part of the brain at the front center, which controls decision making, emotional management, and impulse control.
Type 1 Bipolar: Characterized by mania that is more intense and/or frequent than depression.
Type 2 Bipolar: Characterized by depression that is more intense and/or frequent than hypomania; type 2 bipolar people do not experience "true mania".
*For the sake of this post, "mania" will refer to both hypomania and true mania. When the information only applies to true mania, it will be called "true mania".
----------
Part One: Introduction
We will be exploring the development, behavior, and remission of bipolar brains, using information learned from neuroscience, psychology, and lived experiences of bipolar people. The purpose of this is to inform those with Bipolar how to understand their own brain and take control of the disorder. This post is written by someone diagnosed with Bipolar 2, receiving treatment in the form of medication and talk therapy.
----------
Part Two: Development
This mood disorder usually develops in childhood, but can develop at any point in a person's life. It is caused by trauma, as a response to stress. Most bipolar people also have family with the disorder, implying it is genetically predisposed.
In childhood, this disorder can begin to show symptoms as early as early adolescence. Children as young as 5 have been diagnosed with early onset bipolar disorder.
After traumatic events, such as abuse, neglect, or loss, the brain is forced to find a way to cope and manage complex stress. Trauma can range from mild to severe, and still trigger the onset of bipolar disorder.
During depression, the brain "mines" for dopamine, and during mania, the brain utilizes the dopamine. Over time, without treatment, the bipolar brain will struggle to maintain an effective dopamine-mining system, and these changes will even destroy grey matter in the brain, namely in the prefrontal cortex. This change in the brain makes it more difficult for the prefrontal cortex to communicate with the limbic system, causing less control over emotions and impulses, therefore causing more reckless decisions to be made.
Due to the nature of the relationship between the prefrontal cortex and the limbic system, these two parts of the brain need strong communication. With limited grey matter, signals are weakened, or missed completely.
The hippocampus is a major part of the limbic system, and without a proper connection to send signals between the hippocampus and the prefrontal cortex, it only becomes more difficult to recall past experiences or learned skills.
The longer a bipolar person goes without treatment, the worse their stress, and the worse they respond to stress. This disorder is degenerative, and those with Type 1 Bipolar show the most loss of grey matter.
----------
Part Three: Behavior
Like a pendulum, bipolar brains swing between manic and depressive sensations and behaviors. Here are some characteristics of mood swings:
When depressed, the bipolar person attempts to "fill the void", also known as "dopamine mining". This behavior accumulates dopamine over time but does not release it. This can look like sleeping a lot, escaping into a piece of media, or fixating on an accessible hobby.
During manic swings, the bipolar person uses the dopamine accumulated during depression to compensate for the time lost and labor neglected during depression. This may look like addressing the issue directly in hyper-fixation, or avoiding the issue altogether to indulge in self-pleasure.
Episodes are different than swings. Episodes can be placed on a specific timeframe, sometimes down to the hour. Behaviors are impulsive, emotions are overwhelming, and the decisions made during episodes reflect this heavily. Below are some characteristics of a Bipolar episode, based on type of episode.
In depressive episodes, the bipolar person will display their usual depressive behaviors at a more intense, more frequent rate, and will quickly begin taking on self-destructive behaviors in an effort to punish the self for failing to meet manic expectations. Essentially, the body has gotten used to using depression to recover, and if results are not met, the body "doubles down" as a means to "force" results, in an effort to trigger mania.
Manic episodes are intense highs, often causing changes to the bipolar person's life that normally wouldn't be considered, let alone acted on. There is a false sense of euphoria that controls the impulses and emotions of the bipolar person, causing a disconnect from reality that can lead to delusions and the development of compulsive thoughts or behaviors that enable more poor stress management skills, such as overspending or reckless sexual activity.
Mixed episodes can sometimes be the introduction or ending to a manic or depressive episode, but can also happen alone. The depression attempts to self-destruct while the mania's euphoria makes those behaviors seem euphoric and desirable. These episodes are often painful and typically short-lived compared to the other two, but not necessarily so.
----------
Part Four: Remission
There is a number of ways to treat bipolar brains, though medications and talk therapy, namely CBT and DBT, are the most commonly recommended. Some bipolar brains are medication resistant, so diligent habit seeking and a strong relationship with a therapist may be the best help. Below is an incomplete list of potential treatments, and why they work.
Medication can alter the chemical changes in the brain which trigger swings and episodes. Medication will not heal the brain, it will only control it while properly using the artificial chemicals. Medication plans must be specified to the patient, so trial and error is a necessary process for disordered medicated brains.
Talk therapy flexes the grey matter, and the grey matter may even be recovered in these thought exercises and memory training sessions. These changes are more likely to have a lasting impact, so long as the new habits and beliefs remain.
Diligent habit seeking, centered around self-care and growth, will help a bipolar brain take control of how they treat their stress. While swings may be unavoidable, building a set of healthy habits can alter the way these swings are 'engaged with', meaning behaviors can change. This can be a difficult form of treatment for bipolar people, as the disorder does not consistently provide motivation for habit changes. With a healthy outlook on relapses, this issue is resolved, and habit-seeking can continue even with relapses present.
Healthy coping mechanisms to replace mania are great ways to prevent manic episodes and swings, which will in turn prevent the 'need' for a depressive swing (to recover from manic burnout). These coping mechanisms can look different for each person, but no matter what, these mechanisms must be focused on growth - not escapism, passivity, or indulgence, which are manic behaviors that have been individualized.
Remission looks different for everyone, but no matter what, bipolar is a lifelong disorder. This means that even after years of successful treatment, with no swings or episodes, this disorder is almost guaranteed to make a comeback during high stress situations like abuse or loss. Anyone who has been diagnosed with bipolar should expect to keep their coping mechanisms going for life, and adjusting the mechanisms according to the needs of the changes in their life. There are a few things remission can grant a person, such as:
The ability to work on projects and tasks irregardless of current mood
Motivation to socialize even when the body seeks isolation, making relationships stronger and more consistent
A lack of shame for the disorder or what it has put you through, making stress management less about the desired results and more about the desired process
----------
Part Five: Conclusions
There is no known cure for bipolar disorder, but those with bipolar can take control of their circumstances in small but life changing ways. The bipolar brain is simply trying to thrive even in stressful circumstances, and has only learned one biochemical pattern to do so. Treatment is all about re-training the brain's response to stress. Those who have bipolar must stop identifying with their bipolar to effectively treat it, meaning they cannot embrace their mania as 'the best version of themselves' nor the other way around with their depression. These are not personality traits, because this is not a personality disorder; these are conditions the brain is currently in.
People with bipolar disorder are not to be ashamed of themselves for what they've done to cope during depressive swings or episodes. Shame is often what maintains the cycle, as this is a major driving force of impulsive behavior. The guilt, shame, and self-loathing of a bipolar person will hold them back from developing better ways to manage stress. With an effective, individualized treatment plan, bipolar people can find themselves in remission, but should expect and accept relapse if a major stress is to occur. This is not because the treatment isn't working anymore, but because this is how the brain has developed to respond to stress, and until we find a cure, bipolar brains are to be respected as brains attempting to thrive in unforeseen circumstances - a worthy pursuit that any self-loving person would take on.
----------
Additional notes:
Comorbidity with other mental conditions can cause symptoms to be more intense or more frequent. This includes conditions like PTSD, personality disorders or autism.
Many bipolar people seem to believe that their mania "helps them" - with things like getting projects and tasks done, or socializing. This is false. Mania is what uses the energy accumulated during depression to delude the bipolar person into thinking that the only way for them to get these things done is to indulge in manic behavior. Essentially, the bipolar person is the one helping themselves get their projects and tasks done, and mania is "taking the credit".
If you have been diagnosed with bipolar disorder, you have a strong will to thrive. Trust in this, and rely on that fact to help you change your habits so that your stress management system can adjust to a more stable, secure structure.
You must read the sources for a detailed look at the different topics and ideas shared here. This post is that of my own conclusions, based off of the information in these links plus my own experiences with Bipolar Type 2. I am not a professional, and this post should not be taken as mental health advice, but rather, an exploration from an unprofessional point of view. If you need mental health advice, seek therapy or psychiatric care, and take this information to them to see how it may apply to your life.
----------
Sources:
Bipolar experiences
Dopamine & Bipolar Relationship
Grey matter information
Hippocampus information
Limbic System information
Mania & Hypomania
Mixed episodes
Prefrontal Cortex Walkthrough
#bipolar#bipolar disorder#brain health#bipolar brain#hypomania#mania#depression#manic depression#brain structure#brain development#bipolar episode#mental health#mental healthcare#psychiatry#neuropsychology#psychology#neurology#bipolar treatment#bipolar type 1#bipolar type 2#my essays#my posts
53 notes
·
View notes
Text
I my finally doing my neuropsychology analysis.
There is just something that my afraid: what if they miss something (like this is really expensive)
My psychiatrist suspects autism
My mom suspected ADHD
Like some have any tips on what kind of information I should put on a list?
Does I need to say every embassy anormal thing from my childhood?
--
writing this kinda helped a little bit
4 notes
·
View notes
Text
You think I'm thinking about you but I'm preparing for my neurology exams so I'm thinking about what's next to the Wernicke area in the temporal lobe's neocortex
#moth monologue#psychology#university#college#studying#neuropsychology#neurology#biology#psychblr#stemblr
221 notes
·
View notes
Text
Is the Brain a Driver or a Steering Wheel?
This three part series summarizes what science knows, or thinks it knows, about consciousness. In Part 1 What Does Quantum Physics Imply About Consciousness? we looked at why several giants in quantum physics - Schrodinger, Heisenberg, Von Neumann and others - believed consciousness is fundamental to reality. In Part 2 Where Does Consciousness Come From? we learned the "dirty little secret" of neuroscience: it still hasn't got a clue how electrical activity in the brain results in consciousness.
In this concluding part of the series we will look at how a person can have a vivid conscious experience even when their brain is highly dysfunctional. These medically documented oddities challenge the materialist view that the brain produces consciousness.
Before proceeding, let's be clear what what is meant by "consciousness". For brevity, we'll keep things simple. One way of looking at consciousness is from the perspective of an outside observer (e.g., "conscious organisms use their senses to notice differences in their environment and act on their goals.") This outside-looking-in view is called behavioral consciousness (aka psychological consciousness). The other way of looking at it is the familiar first-person perspective of what it feels like to exist; this inside-looking-out view is called phenomenal consciousness (Barušs, 2023). This series is only discussing phenomenal consciousness.
Ready? Let’s go!

Source: Caltech Brain Imaging Center
A Hole in the Head
Epilepsy is a terrible disease in which electrical storms in the brain trigger seizures. For some people these seizures are so prolonged and frequent that drastic action is needed to save their lives. One such procedure is called a hemispherectomy, the removal or disconnection of half the brain. Above is an MRI image of a child who has undergone the procedure.
You might think that such radical surgery would profoundly alter the memory, personality, and cognitive abilities of the patient.
You would be wrong. One child who underwent the procedure at age 5 went on to attend college and graduate school, demonstrating above average intelligence and language abilities despite removal of the left hemisphere (the zone of the brain typically identified with language.) A study of 58 children from 1968 to 1996 found no significant long-term effects on memory, personality or humor, and minimal changes in cognitive function after hemispherectomy.
You might think that, at best, only a child could successfully undergo this procedure. Surely such surgery would kill an adult?
You would be wrong again. Consider the case of Ahad Israfil, an adult who suffered an accidental gunshot to the head and successfully underwent the procedure to remove his right cerebral hemisphere. Amazingly, after the five hour operation he tried to speak and went on to regain a large measure of functionality (although he did require use of a wheelchair afterwards.)
Another radical epilepsy procedure, a corpus collosotomy, leaves the hemispheres intact but severs the connections between them. For decades it was believed that these split-brain patients developed divided consciousness, but more recent research disputes this notion. Researchers found that, despite physically blocking all neuronal communication between the two hemispheres, the brain somehow still maintains a single unified consciousness. How it manages this feat remains a complete mystery. Recent research on how psychedelic drugs affect the brain hints that the brain might have methods other than biochemical agents for internal communication, although as yet we haven't an inkling as to what those might be.
So what's the smallest scrape of brain you need to live? Consider the case of a 44-year-old white collar worker, married with two children and with an IQ of 75. Two weeks after noticing some mild weakness in one leg the man went to see his doctor. The doc ordered a routine MRI scan of the man's cranium, and this is what it showed.
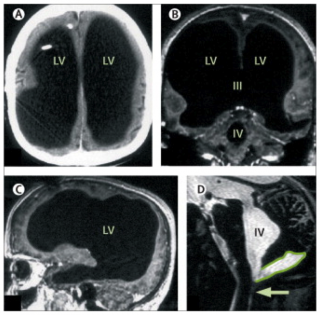
Source: The Lancet
What you are seeing here is a giant empty cavity where most of the patient's brain should be. Fully three quarters of his brain volume is missing, most likely due to a bout of hydrocephalus he experienced when he was six months old.

Last Words
Many unusual phenomena have been observed as life draws to an end. We're going to look at two deathbed anomalies that have neurological implications.
The first is terminal lucidity, sometimes called paradoxical lucidity. First studied in 2009, terminal lucidity refers to the spontaneous return of lucid communication in patients who were no longer thought to be medically capable of normal verbal communication due to irreversible neurological deterioration (e.g., Alzheimers, meningitis, Parkinson's, strokes.) Here are three examples:
A 78-year-old woman, left severely disabled and unable to speak by a stroke, spoke coherently for the first time in two years by asking her daughter and caregiver to take her home. She died later that evening.
A 92-year-old woman with advanced Alzheimer’s disease hadn’t recognized her family for years, but the day before her death, she had a pleasantly bright conversation with them, recalling everyone’s name. She was even aware of her own age and where she’d been living all this time.
A young man suffering from AIDS-related dementia and blinded by the disease who regained both his lucidity and apparently his eyesight as well to say farewell to his boyfriend and caregiver the day before his death.
Terminal lucidity has been reported for centuries. A historical review found 83 case reports spanning the past 250 years. It was much more commonly reported in the 19th Century (as a sign that death was near, not as a phenomenon in its own right) before the materialist bias in the medical profession caused a chilling effect during the 20th Century. Only during the past 15 years has any systematic effort been made to study this medical anomaly. As a data point on its possible prevalence a survey of 45 Canadian palliative caregivers found that 33% of them had witnessed at least one case of terminal lucidity within the past year. Other surveys found have that the rate of prevalence is higher if measured over a longer time window than one year, suggesting that, while uncommon, terminal lucidity isn't particularly rare.
Terminal lucidity is difficult to study, in part because of ethical challenges in obtaining consent from neurocompromised individuals, and in part because its recent identification as a research topic presents delineation problems. However, the promise of identifying new neurological pathways in the brains of Alzheimer's and Parkinson's patients has gotten a lot of attention. In 2018 the US National Institute on Aging (NIA) announced two funding opportunites to advance this nascent science.
Due to the newness of this topic there will continue be challenges with the data for some time to come. However, its impact on eyewitnesses is indisputably profound.

Near Death Experiences
The second deathbed anomaly we will take a look at are Near-Death Experiences (NDEs.) These are extraordinary and deeply personal psychological experiences that typically (but not always) occur during life-threatening emergencies such as cardiac arrest, falls, automobile accidents, or other traumatic events; they are also occasionally reported during general anesthesia. Much of the research in this area has focused on cardiac arrest cases because these patients are unconscious and have little to no EEG brain wave activity, making it difficult to account for how the brain could sustain the electrical activity needed to perceive and remember the NDE. This makes NDEs an important edge case for consciousness science.
NDEs are surprisingly common. A 2011 study published by the New York Academy of Sciences estimated that over 9 million people in the United States have experienced an NDE. Multiple studies have found that around 17% of cardiac arrest survivors report an NDE.
There is a remarkable consistency across NDE cases, with experiencers typically reporting one or more of the following:
The sensation of floating above their bodies watching resuscitation efforts, sometimes able to recall details of medical procedures and ER/hallway conversations they should not have been aware of;
Heightened sensations, occasionally including the ability of blind and deaf people to see and hear;
Extremely rapid mental processing;
The perception of passing through something like a tunnel;
A hyper-vivid life review, described by many experiencers as "more real than real";
Transcendent visions of an afterlife;
Encounters with deceased loved ones, sometimes including people the experiencer didn’t know were dead; and
Encounters with spiritual entities, sometimes in contradiction to their personal belief systems.
Of particular interest is a type of NDE called a veridical NDE. These are NDEs in which the experiencer describes events that occurred during the period when they had minimal or no brain activity and should not have been perceived or remembered if the brain were the source of phenomenal consciousness. These represent about 48% of all NDE accounts (Greyson 2010). Here are a few first-hand NDE reports.
A 62-year-old aircraft mechanic during a cardiac arrest (from Sabom 1982, pp. 35, 37)
A 23-year-old crash-rescue firefighter in the USAF caught by a powerful explosion from a crashed B-52 (from Greyson 2021, pg. 27-29)
An 18-year-old boy describes what it was like to nearly drown (from the IANDS website)
There are thousands more first person NDE accounts published by the International Association for Near-Death Studies and at the NDE Research Foundation. The reason so many NDE accounts exist is because the experience is so profound that survivors often feel compelled to write as a coping method. Multiple studies have found that NDEs are more often than not life-changing events.
A full discussion of NDEs is beyond the scope of this post. For a good general introduction, I highly recommend After: What Near-Death Experiences Reveal about Life and Beyond by Bruce Greyson, MD (2021).

The Materialist Response
Materialists have offered up a number of psychological and physiological models for NDEs, but none of them fits all the data. These include:
People's overactive imaginations. Sabom (1982) was a skeptical cardiologist who set out to prove this hypothesis by asking cardiac arrest survivors who did not experience NDEs to imagine how the resuscitation process worked, then comparing those accounts with the veridical NDE accounts. He found that the veridical NDE accounts were highly accurate (0% errors), whereas 87% of the imagined resuscitation procedures contained at least one major error. Sabom became convinced that NDEs are real. His findings were replicated by Holden and Joesten (1990) and Sartori (2008) who reviewed veridical NDE accounts in hospital settings (n = 93) and found them to be 92% completely accurate, 6% partially accurate, and 1% completely inaccurate.
NDEs are just hallucinations or seizures. The problem here is that hallucinations and seizures are phenomena with well-defined clinical features that do not match those of NDEs. Hallucinations are not accurate descriptions of verifiable events, but veridical NDEs are.
NDEs are the result of electrical activity in the dying brain. The EEGs of experiencers in cardiac arrest show that no well-defined electrical activity was occurring that could have supported the formation or retention of memories during the NDE. These people were unconscious and should not have remembered anything.
NDEs are the product of dream-like or REM activity. Problem: many NDEs occur under general anesthesia, which suppresses dreams and REM activity. So this explanation cannot be correct.
NDEs result from decreased oxygen levels in the brain. Two problems here: 1) The medical effects of oxygen deprivation are well known, and they do not match the clinical presentation of NDEs. 2) The oxygen levels of people in NDEs (e.g., during general anesthesia) has been shown to be the same or greater than people who didn’t experience NDEs.
NDEs are the side effects of medications or chemicals produced in the brain (e.g. ketamine or DMT). The problem here is that people who are given medications in hospital settings tend to report fewer NDEs, not more; and drugs like ketamine have known effects that are not observed in NDEs. The leading advocate for the ketamine model conceded after years of research that ketamine does not produce NDEs (Corraza and Schifano, 2010).

Summing Up
In coming to the end of this series, let's sum up what we discussed.
Consciousness might be wired into the physical universe at fundamental level, as an integral part of quantum mechanics. Certainly several leading figures in physics thought so - Schrodinger, Heisenberg, Von Neumann, and more recently Nobel Laureate Roger Penrose and Henry Stapp.
Materialist propaganda notwithstanding, neuroscience is no closer to identifying Neural Correlates of Consciousness (NCCs) than it was when it started. The source of consciousness remains one of the greatest mysteries in science.
Meanwhile, medical evidence continues to pile up that there is something deeply amiss with the materialist belief that consciousness is produced by the brain. In a sense, the challenge that NDEs and Terminal Lucidity pose to consciousness science is analogous to the challenge that Dark Matter poses to physics, in that they suggest that the mind-brain identity model of classic materialist psychology may need to be rethought to adequately explain these phenomena.
Ever since the Greeks, science has sought to explain nature entirely in physical terms, without invoking theism. It has been spectacularly successful - particularly in the physical sciences - but at the cost of excluding consciousness along with the gods (Nagel, 2012). What I have tried to do in this series is to show that a very credible argument can be made that materialism has the arrow of causality backwards: the brain is not the driver of consciousness, it's the steering wheel.
I don't think we are yet ready to say what consciousness is. Much more research is needed. I'm not making the case for panpsychism, for instance - but I do think consciousness researchers need to throw off the assumption drag of materialism before they're going to make any real progress.
It will be up to you, the scientists of tomorrow, to make those discoveries. That's why I'm posting this to Tumblr rather than an academic journal; young people need to hear what's being discovered, and the opportunities that these discoveries represent for up and coming scientists.
Never has Planck's Principle been more apt: science advances one funeral at a time.
Good luck.
For Further Reading
Barušs, Imants & Mossbridge, Julia (2017). Transcendent Mind: Rethinking the Science of Consciousness. American Psychological Association, Washington DC.
Barušs, Imants (2023). Death as an Altered State of Consciousness: A Scientific Approach. American Psychological Association, Washington DC.
Batthyány, Alexander (2023). Threshold: Terminal Lucidity and the Border of Life and Death. St. Martin's Essentials, New York.
Becker, Carl B. (1993). Paranormal Experience and Survival of Death. State University of New York Press, Albany NY.
Greyson, Bruce (2021). After: A Doctor Explores What Near-Death Experiences Reveal about Life and Beyond. St. Martin's Essentials, New York.
Kelly, Edward F.; Kelly, Emily Williams; Crabtree, Adam; Gauld, Alan; Grosso, Michael; & Greyson, Bruce (2007). Irreducible Mind: Toward a Psychology for the 21st Century. Rowman & Littlefield, New York.
Moody, Raymond (1975). Life After Life. Bantam/Mockingbird, Covington GA.
Moreira-Almeida, Alexander; de Abreu Costa, Marianna; & Coelho, Humberto S. (2022). Science of Life After Death. Springer Briefs in Psychology, Cham Switzerland.
Penfield, Wilder (1975). Mystery of the Mind: A Critical Study of Consciousness and the Human Brain. Princeton Legacy Library, Princeton NJ.
Sabom, Michael (1982). Recollections of Death: A Medical Investigation. Harper and Row Publishers, New York.
van Lommel, Pim (2010). Consciousness Beyond Life: The Science of the Near-Death Experience. HarperCollins, New York.
#consciousness#cognitive science#near death experiences#nde#terminal lucidity#terminal illness#cognitive neuroscience#paradoxical lucidity#hemispherectomy#corpus collosotomy#psychadelic#psychonaut#psychonauts#psilocybin#lsd#ketamine#materialism and its discontents#neurology#neuropsychology#philosophy of mind#brain#quantum physics#consciousness series
51 notes
·
View notes
Text
There are about 180 billion nerve cells (neurons) in the human brain, and each one communicates with several or even tens of thousands of other nerve cells
63 notes
·
View notes
Text
Metacognitive Awareness Study
Hello everyone, I'm seeking research participants for my counseling psychology dissertation project.
This research was inspired by prior research which suggests autistic cognition, is biased in general towards local or detail focused style over a global or gestalt.
This led to thinking about how people use compensation strategies to overcome challenging situations which in part can contribute to late identification/diagnosis and also masking which has a poor impact on autistic people's mental health.
If anyone is interested in participating it is open to all, non-autistic, autistic and self-identifying people.
Requires:
~ 30 minutes
– Must be over 18 years old
– Demographics and Screening Survey
– Facial emotions and eye color task
– Metacognition questionnaire
– Won't work on most mobile devices
– Not paid – Sorry!
Thanks for reading.
Direct link:

#psychology#metacognition#autism#actually autistic#mentalhealth#cognition#actuallyautistic#creativity#cognitivepsychology#masking#ADHD#Neurodiversity#Neurodivergent#dyslexia#learningdifficulties#sensory issues#audhd#neurodivergence#neurospicy#neuroscience#neuropsychology
2 notes
·
View notes