#mucormycosis black fungus
Text
Black Fungus; Definition, Symptoms and Causes
Black Fungus or Mucormycosis is a disease that is caused by a Fungus called Mucormycetes. This fungus is commonly found in our environment. Although the incidence of this disease is not new, it is a challenge that the Fungus attack is common to COVID-19 Patients. And it is a serious fungal infection that can affect our eyesight and even the brain.
Symptoms
According to the United States Center…

View On WordPress
0 notes
Note
I saw your tags on the mycology tumblr post - I challenge you to scare me with a mushroom fact. I’ve harvested and eaten wild mushrooms a few times, I’ve got my share of guidebooks and worked on research my university did on suede boletes. I’m no spring chicken of the woods but i’m also far from an expert. Scare me with the Deep Mushroom Lore
Woaaaah this got a bit lost and im a bit late, yikes! Anyway it looks like you were focusing on the Basidiomycota phylum which is where a lot of the frontliners and popular ones are. But let's look at the Ascomycota, lots of scary stuff there, lord there's so much but baseline ig is cordyceps which everyone knows about now. They can alter and control insects, a big example is bullet ant behavior to makes them climb as high as they can and bite onto the grass or whatnot to secure themselves until the host dies. They go as high as possible so when the cordycep actually grows the fruitbody the spores can spread as far as possible. Luckily for us human nervous systems are way too complex for the cordyceps....for now.

I mean any parasite that controls it's host is crazy and I 10000% recommend looking into it.
There's another fungus Laboulbeniomycetes that grows exclusively on arthropod exoskeleton.

A lot of fungal diseases make me shudder, there are probably fungal spores in your lungs right now! Pneumocystis is the genus of a yeast that loves your lungs and you guessed it, causes a strain of pneumonia that's very hard to diagnose! Yippee! Mostly because it is very hard to culture.
Let's look at everyone's favorite yeast Conidida. This guy is DIMORPHIC so it can be a yeast or invasive hyphae depending on environmental triggers/conditions, and wouldn't you know it, lives at human body temp. This guy causes yeast infections and the like.
Aspergillus is one that ferments soy products BUT can also cause Apergillosis which can cause an allergic reaction and eventually a fungal ball growth in your lungs, aak!
In a different phylum, Mucoromycota, Mucormycosis is probably my least favorite as the group USUALLY targets your fruits and is that pesky mold. Well another version of it will target the sinuses of immunocompromized diabetics. These are sugar loving molds so uhhhhh, no bueno. I recommend looking at pictures with CAUTION it is gross. The eyes can get really messed up, black lesions can show up on your face really really nasty stuff.
Anyway, Ascomycota cool group, lots of human diseases (many of which are hard to cure because of how close fungi are to animals so we target very specific things in their cells but OOPS resistance is on the rise), have fun with this info ::)
#mycology#ascomycota really popped off on the diseases#ollie rambles#<<<yea no i RAMBLED#but yea apologies for how late this is been reaaaally busy#long post#call me patient zero the way fungi have consumed my mind
23 notes
·
View notes
Text
Rhizopus & Mucor
Both belong under the umbrella term, mucorales.
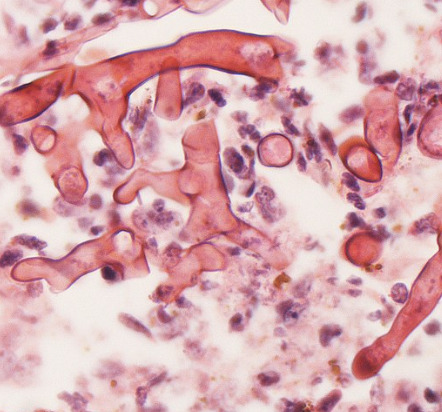
These are bread moulds naturally on fruit and bread that we breathe in and out without much issue particularly if immunocompetent, but in some immunocompromised it causes rapidly fatal and progressive disease: mucormycosis. Due to the weakened immune system.

Spores released either land on skin or into blood via open wounds, then deposit tehre, invading local vessels, thrombosing them and cutting off supply. this rapidly leads to ischaemia and necrosis. Dead tissue.
Now for a Case Report.
This one in Frontiers of Medicine. A 35 yo man with diabetes presents with a facial rash, that rapidly progresses to an eschar and ulcer. To note, there are graphic images in the link of his face.
This was initially associated with nasal discharge and epistaxis. Diagnosis was initially a peridontal infection which did not resolve with standard antibiotics for this, similarly he was next diagnosed with uncomplicated, stock standard cellulitis (usually staph or strep pyogenes caused). Both treatments failed.
eventually he was diagnosed with mucormycosis, but by then he had extensive damage to his face, the subcut tissues, muscles and facial bones. He also had significant weight loss, fevers, splenomegaly and thrombosis.
To muddy the waters, he was concurrently diagnosed with a T cell lymphoma but the authors also picked up Rhizopus.
What is Rhizopus? (also related to mucor, another mucorales)
It's a fungi, more specifically an opportunistic pathogen commonly associated with diabetics (esp poorly controlled) and the immunocompromised (in particular solid organ transplants, see further case report in resources below, HIV, malnutrition, haematological malignancies - eg leukaemias).
Also associated with steroid use, form of immunosuppression so has been seen in severe COVID patients requiring dexamethasone (Rare though).
As a mould it likes the acidotic states in DKA and iron, so any iron overload states as well.
Why poorly controlled diabetics - it becomes an immunocormposed state in and of itself. The sugars suppress local inflammatory responses like neutrophil chemotaxis or phagocytosis etc.
You can however, get chronic forms too. So don't rule it out if it's not wildly acute. These occur over weeks, slowly.
Considering it's a mould, it's particularly "prolific" in hot weather and warm/hot climates.
Classically it is an infection that affects the face, parasinuses, nose and even the brain. You'll often hear the term rhinocerebral with it.
Consider it if you see discolouration around the face and definitely if you see a necrotic eschar. Actually, any black spots, fevers, rash, call ID urgently. Unsurprisingly, it is also called the black fungus.

Is also possible to have it affect the skin (particularly in IVDU and in burns), lungs and GI (more rare). IN lung involvement symptoms are typical for the organ - SOB, fevers, chest pain, haemoptysis. in GI: nausea/vomiting/GIB.
Thrombosis can occur as a complication as it invades the blood vessels.
In brain involvement from disseminated disease, expect confusion and altered state if not reduced GCS.
It's also been recently featured in the fungi podcast by the Curbsiders. Which is worth a listen.
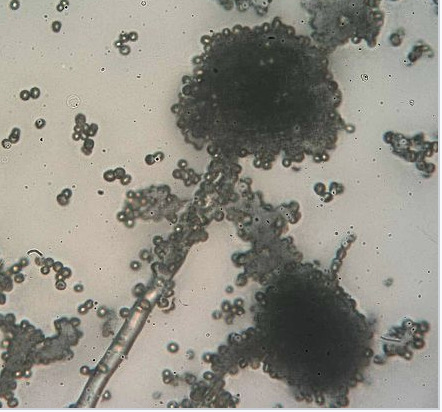
It's filamentous and has hyphae.
You'll also hear the term mucormycosis = which just refers to the disease process that is rapidly fatal. Mortality is 30-70% of rhinocerebral cases, 90% in disseminated and 100% in AIDs --numbers from StatPearls. Survival improves with antifungals and surgery to 70%.
Early diagnosis and intervention is essential, as illustrated in the case report above. but is rare, so not infrequently missed.
It's also missed, as early symptoms are very non specific depending on how it affects the host. You can simply get lethargy, headache and eye pain. Blurry vision too, or simply epistaxis and rhinorrhoea.
Image from Wiki
Now that you know the clinical presentation and the increased risk groups to think of this diagnosis in,
How do you confirm your suspicions?
investigations:

It's associated with neutropaenic states and one hypothesis is acidosis in diabetics with poorly managed sugars (so really unwell). No serology (as compared to other bugs), would come up in fungal cultures and on tissue biopsy. key words on biopsy: Ribbon like hyphae branching at 90 degree angles.
Also from wiki, that suggests it looks like Moose antlers.

Pathologists will also note or look for necrosis and haemorrhage.
Blood cultures rarely pick up it, so consider it if they're unwell and culture negative.
On imaging - gold standard in rhino cerebral is MRI but CT is most accessible and fast. Looking for signs of blood vessel invasion and reverse halo or less specific halo sign.
Reverse halo per radiopaedia: ground glass within a consolidated crescent shape.
From radiopaedia:

Okay, this sounds both difficult to pick up and investigate. No magical PCR or serology.
Pro tip from stat pearls: just maintain a high index of suspicion in anyone with increased risk or risk factors. Biopsy tissue quickly particularly if necrosis is apparent. Early detection method is unsurprisngly CT --> we all seem to have a low threshold for this, but looking for hyperdensity (mucosal thickening) and erosion of the facial bones.
Also essential is the age old adage that most clinicians follow --> empirical therapy for the most common organisms, close monitoring/observations. then failing that, broaden the differentials and keep investigating or altering treatment quickly.
Treatment:
The strong stuff. Liposomal Amphotericin B for 4-6 weeks (the long duration) as it is highly invasive/progressive. Alternatives; itraconazole.
You may also hear of hyperbaric O2 therapy, which aids the neutrophils to kill the fungi. Also in stat pearls
Surgical debridement after antifungal therapy with washout depending on extent of damage.
Sources used for post:
Case reports, wiki and radiopaedia as above
And largely Statpearls --> there is much more further detail and more to read on differentials and complications.
I'll try to use free resources as much as possible.
Another Case Reports of interest include: NEJM - lengthy one reminding all to consider this diagnosis in an unexplained rash in an immunocompromised host.
5 notes
·
View notes
Text
Mucormycosis (research post)

Mucormycosis is also known as ‘black fungus’ and it is a very serious and rare fungal infection
How is it caused?:
Mucormycetes are a type of mold that is present in our environment, usually in soil and organic matter in the process of decay (i.e compost).
Usually coming into contact with this type of mold is harmless, however mucormycosis typically presents in people with compromised immune systems.
There are five different types of mucormycosis:
Pulmonary mucormycosis (Infection of the lung)
Gastrointestinal mucormycosis (Infection of the GI tract)
Cutaneous mucormycosis (Infection of the skin)
Disseminated mucormycosis (Infection spread through the bloodstream)
Symptoms: The symptoms may vary for each type of mucormycosis however it generally presents as a respiratory or skin infection
Fever
Headache
Cough
Nasal congestion
Sinus pain
Swelling
Redness
Blisters
Ulcers
Blackened skin tissue
Treatment:
Mucormycosis is treated with a prescription antifungal medication, and is usually given intravenously or orally. The primary medication given is isavuconazole. However amphotericin B or posaconazole can also be administered depending on the patient's requirements.
___
Note: Second post and all I can say is....wow. This was a bit scary to think about how doing something as normal as like hanging around in a park or playing in the grass and soil could lead to something so detrimental, stay safe everyone. Here's another badly made meme that I couldn't stop laughing at for some reason- and I hope you all have an amazing day!

0 notes
Text
Mucormycosis, also known as black fungus, is a rare but serious fungal infection that has recently emerged as a post-COVID complication in some patients. Proper mucormycosis treatment is crucial given its high mortality rates and the limited timeline...
#Mirari #MirariDoctor #MirariColdPlasma #ColdPlasma
0 notes
Text
0 notes
Text
Dr. Abhishek Kumar Sinha, Dermatologist in Patna- Unmasking the Most Serious Fungal Infection-

Title: Unmasking the Most Serious Fungal Infection: Insights from Dr. Abhishek Kumar Sinha, Dermatologist in Patna
Fungal infections come in various forms, and while most are relatively mild and treatable, some can pose serious health risks. Dr. Abhishek Kumar Sinha, a respected dermatologist in Patna, aims to create awareness among the general population about the most serious fungal infection.
One of the most alarming fungal infections is invasive aspergillosis, caused by the Aspergillus species. This infection primarily affects individuals with weakened immune systems, such as those undergoing chemotherapy or organ transplant recipients. Invasive aspergillosis can be life-threatening, as it invades the lungs and can spread to other organs, leading to severe respiratory distress and systemic complications.
Another serious fungal infection is mucormycosis, often referred to as the "black fungus." It can occur in individuals with uncontrolled diabetes, compromised immune systems, or those who have recently recovered from COVID-19. Mucormycosis rapidly spreads through the bloodstream, causing tissue necrosis and damage to vital organs.
Cryptococcal meningitis is also a severe fungal infection, mainly affecting individuals with advanced HIV/AIDS. It invades the central nervous system and can lead to life-threatening neurological complications.
While these infections are indeed serious, it's crucial to remember that prompt diagnosis and appropriate medical intervention can significantly improve the chances of recovery. If you or a loved one experience symptoms such as persistent fever, severe headache, breathing difficulties, or changes in mental status, seek immediate medical attention.
In conclusion, the most serious fungal infections often target individuals with weakened immune systems. Awareness of these infections and early medical intervention are essential for better outcomes. Consult with a healthcare professional like Dr. Abhishek Kumar Sinha for accurate diagnosis and treatment if you suspect a severe fungal infection.
0 notes
Text
https://www.secondmedic.com/blogs/treating-black-fungus-how-is-mucormycosis-treated
0 notes
Text
Enhancing Vision and Care: EyeSite Eye Hospital and Retina Centre
Introduction :
In the realm of eye care, precision and expertise are paramount. When it comes to your vision, you deserve nothing less than the best. That's where EyeSite Eye Hospital and Retina Centre in Indore shines. As a super speciality hospital in Indore, we are committed to providing world-class eye care services. Our team of dedicated specialists caters to a wide range of eye conditions, including retina-related issues, cataracts, and more. In this blog, we will explore our commitment to excellence and how we are making a significant impact on eye health in Indore.
Retina: The Core of Our Expertise :
The retina, a delicate tissue at the back of the eye, is essential for clear vision. At EyeSite Eye Hospital and Retina Centre, we specialize in diagnosing and treating a multitude of retinal disorders. Our experienced eye specialists in Indore employ state-of-the-art techniques, such as Fundus Fluorescein Angiography (FFA), to precisely assess and manage retinal conditions.
Types of Cataracts: Understanding the Clouding of Vision :
Cataracts, a common eye ailment, can significantly impair your vision. There are various types of cataracts, each affecting different parts of the eye lens. Our Indore hospital offers comprehensive cataract care, addressing conditions like nuclear cataracts, cortical cataracts, and subcapsular cataracts. With advanced surgical techniques, we can remove cataracts and restore your vision effectively.
Eye Care in Indore: My Hospital, Your Vision :
EyeSite Eye Hospital and Retina Centre takes pride in being your trusted "my hospital" in Indore. Our commitment to excellence, compassionate care, and a patient-centric approach have made us a top choice for eye health in the region. Whether you're seeking general eye care or specialized treatments, our team of eye specialists in Indore is here to ensure your vision is in the best hands.
The Essence of Our Eye Hospital in Indore :
Our eye hospital in Indore is more than just a medical facility; it's a place where vision meets innovation. As one of the NABH-accredited hospitals in the region, we adhere to the highest standards of patient care and safety. We employ cutting-edge technologies, such as Fundus Fluorescein Angiography (FFA), to provide accurate diagnoses and treatments for various eye conditions.
Eye Angiogram: A Window to Eye Health :
Fundus Fluorescein Angiography (FFA), commonly known as an eye angiogram, is a diagnostic tool that allows us to visualize the blood vessels in your retina. This procedure helps us detect and manage retinal disorders effectively. At EyeSite Eye Hospital and Retina Centre, we offer FFA as part of our comprehensive retinal care services, ensuring that your eye health is thoroughly evaluated and treated.
The Challenge of Black Fungus and Eye Health :
In recent times, the emergence of black fungus (Mucormycosis) has raised concerns, particularly regarding its impact on the eyes. Our experienced team is well-prepared to address black fungus eye cases, providing timely and expert care to protect your vision. Early diagnosis and treatment are critical, and we are equipped to handle these challenging cases with precision.
Eye Health Tips: Preserving Your Precious Vision :
At EyeSite Eye Hospital and Retina Centre, we not only treat eye conditions but also promote proactive eye health. Here are some valuable eye health tips to help you maintain optimal vision:
1. Regular Eye Check-ups: Schedule routine eye examinations to detect issues early.
2. Healthy Diet: Consume foods rich in vitamins and antioxidants to support eye health.
3. UV Protection: Wear sunglasses with UV protection to shield your eyes from harmful sun rays.
4. Hydration: Stay well-hydrated to prevent dry eyes.
5. Screen Time: Limit screen time and take breaks to reduce digital eye strain.
Conclusion:
EyeSite Eye Hospital and Retina Centre in Indore stands as a beacon of hope for those seeking comprehensive eye care. From retina-related concerns to cataracts and more, our super speciality hospital is equipped with the expertise and technology needed to preserve and restore your vision. When you think of "eye specialist in Indore" or "eye hospital in Indore," think of us as your dedicated partner in eye health. Your vision is our priority, and we are here to ensure it remains clear and vibrant.
0 notes
Text
How to Treat & Prevent Fungal Infections in Humid Weather
In Kuwait, where the humid weather can foster the establishment spread of fungal diseases, it is essential to be aware of the risks posed by conditions like athlete's foot, ringworm, and yeast infections.
Fungi thrive in warm, damp environments, making it crucial for individuals to take proper precautions when faced with these common ailments.
If you experience any symptoms or concerns related to fungal infections, it is advisable to visit a reputable dermatology clinic in Kuwait to receive expert care and guidance for managing these conditions effectively.
In this post, we will talk about fungal infections and present some helpful strategies for preventing your skin from fungus in humid conditions.
What are Fungal Infections?
Fungal infections, often known as mycosis, are illnesses caused by fungi (yeast or mold).
Fungal infections commonly occur on the skin or nails, but fungi (plural of fungus) can also lead to infections in various parts of your body, including the mouth, throat, lungs, urinary tract, and other regions.
Types, Symptoms, and Causes of Fungal Infections
1. Athlete's Foot
Symptoms: Itchy, red, and scaly skin between toes
Causes: Fungi called dermatophytes, often found in warm, moist environments like public showers or swimming pools.
2. Yeast Infections
Symptoms: Vaginal itching and discharge
Causes: Candida albicans, a type of yeast that naturally resides in the body and can overgrow in certain conditions.
3. Ringworm
Symptoms: Circular, red, and itchy patches on skin
Causes: Dermatophytes, similar to those causing athlete's foot, transmitted through contact with an infected person.
4. Jock Itch
Symptoms: Itchy and red groin area
Causes: Dermatophytes, commonly transmitted through contact with contaminated objects or infected individuals.
5. Aspergillosis
Symptoms: Fever, cough, and shortness of breath
Causes: Inhalation of Aspergillus spores found in the environment, especially affecting those with weak immune systems.
6. Histoplasmosis
Symptoms: Flu-like symptoms, chest pain, and joint pain
Causes: Inhalation of Histoplasma capsulatum spores found in soil enriched with bird or bat droppings.
7. Mucormycosis
Symptoms: Facial pain, black lesions on nasal bridge
Causes: Inhalation of Mucorales fungal spores commonly found in soil and decaying organic matter.
8. Blastomycosis
Symptoms: Fever, cough, and muscle aches
Causes: Inhalation of Blastomyces dermatitidis spores found in soil enriched with decomposing organic materials.
The Most Common Risk Factors for Fungal Infections
Living in hot and humid regions, sweating excessively, or wearing moist clothing can all lead to the development of fungal infections.
Fungal infections can be caused by weakened immunity due to underlying disorders such as diabetes, HIV, cancer, etc.
Living in a dirty environment and failing to maintain personal hygiene might lead to fungal diseases.
Wearing dirty garments, such as soiled socks and innerwear, can lead to fungal infections.
Tight clothing can create sweat, which provides the required moisture for fungus to develop quickly.
Obesity can result in fungal infections. Moisture can be trapped in skin creases, providing a breeding habitat for fungus.
Stress can further erode our immunity, leading to fungal infections.
Hormonal changes can cause vaginal infections during pregnancy.
Practical Tips for Protecting Your Skin Against Fungal Infections
1. Maintain clean, dry skin
To avoid fungal infections, maintaining excellent cleanliness is essential.
Cleanse your skin thoroughly, paying specific attention to regions like your feet, groin, and armpits prone to sweat collection.
Dry these areas entirely after showering or exercising to avoid moisture accumulation.
If you notice any unusual skin conditions or persistent issues, its essential to seek advice from a qualified skin doctor in Kuwait to get a proper diagnosis and treatment
2. Put on breathable garments
Choose lightweight, breathable textiles like cotton or linen that promote air circulation and absorb sweat.
Avoid wearing clothing that is too tight and traps moisture against the skin since this creates an excellent habitat for fungus to develop.
3. Make use of antifungal powders
Antifungal powders can help absorb moisture and suppress fungus development, especially in sweaty areas.
Pay specific care to your feet, as they are prone to ailments such as athlete's foot.
Sprinkle antifungal powder on your shoes and socks to keep your feet dry and clear of fungal diseases.
4. Avoid walking barefoot in public places
Fungal infections are quickly disseminated by contact with contaminated surfaces, such as public showers, swimming pools, and changing rooms.
Wear flip-flops or water-resistant sandals whenever possible in these areas to reduce direct contact and the potential of developing fungus.
5. Avoid sharing personal items
Sharing personal items such as towels, clothing, or shoes may facilitate the fungus spread.
To avoid cross-contamination, use only your personal items and do not give them to anybody else, not even close relatives.
6. Look for prompt treatments
It is essential to get medical attention as soon as you suspect a fungal infection or see signs on your skin, such as redness, itching, or a rash.
Seek therapy from a certified skin doctor in Kuwait. Fungal skin lesions should be carefully recognized and treated accordingly.
Adherence to the suggested treatment plan is essential for optimal recovery.
Way Forward
Fungal infections are more common in humid regions, but following these measures and employing effective treatment procedures may dramatically reduce your chances of acquiring or spreading such diseases.
Always keep your skin dry, practice good hygiene, and seek expert advice from a dermatology clinic in Kuwait when required.
Even in humid conditions, you may live comfortably and healthily by taking preventive precautions.
If you experience any of these symptoms and want to inquire about them, speak to our dermatologists at Quttainah Medical Center in Kuwait to learn more.
0 notes
Link
0 notes
Text
Sinusitis Relief with Home Remedies | MedyBlog

Fighting with sinusitis is about maintaining a balance between infection and immunity. Our body can fight out the infection in acute sinusitis with good immunity. When the body does not control acute sinusitis, it progresses to chronic sinusitis. Immunity alone cannot fight chronic sinusitis. Our immunity is the only fighter against any infection, and antibiotics or antifungal are weapons that empower our immunity.
Home Remedies-
1. Small but many workouts daily
2. Steam inhalation
3. Magical immunity booster combination for sinusitis relief
4. Stay hydrated
5. Adequate sleep
So, adding supportive Home Remedies to Relieve Sinus Pressure to acute sinusitis can prevent the transition to the chronic stage and provide relief.
#symptoms of middle ear infection#sinus cause ear infection#home remedies to relieve sinus pressure#ear infection#mucormycosis curable#black fungus curable#acute on chronic sinusitis#acute sinus infection symptoms#severe sinus ear pain#Problems with Sinuses#Aspergillus Niger#fungal ear infection
0 notes
Text
What is the treatment of Black Fungus?
Everyone loves their life and wants to keep their health good. To keep their health good, they have to keep their lifestyle good. Now, some things have to be done to keep the lifestyle good, such as physical activity, yoga, meditation, exercise, a healthy diet, sleeping early, getting up early, and keeping yourself away from habits like drugs. When you have a good lifestyle, it means that you are living a healthy life. A good lifestyle keeps your health strong, keeps your immunity strong, keeps you mentally strong, and also strengthens your willpower. Today we will talk about the disease black fungus and the treatment of black fungus, which is also known as "Mucormycosis".
Read more
0 notes
Text
Molecular Docking studies on the Anti-fungal activity of Allium sativum (Garlic) against Mucormycosis (black fungus) by BIOVIA discovery studio visualizer 21.1.0.0
Background: The COVID-19 pandemic is a major concern. However, its association and rising cases of mucormycosis, also known as black fungus make the scenario even more troublesome. In addition, no specific medication against mucormycosis/black fungus makes things even worse.
Objective: Garlic phytoconstituents have shown remarkable antifungal properties against various fungal species in various studies. Thus, the objective of the study was to check the potency of garlic phytoconstituents against the 1,3-beta-glucan synthase fungal protein using in-silico methods.
Method: Auto Dock was used to evaluate selected garlic phytochemical molecules against 1,3-beta-glucan synthase fungal protein, and Discovery studio visualizer was used to create 3D and 2D interaction photos.
Results: Five out of 9 phytoconstituents were found to form conventional hydrogen bonds, and only alliin formed the highest number of hydrogen bonds. However, the binding energy and inhibition constant of all nine phytoconstituents were determined. Interestingly, Z-ajoene showed the lowest binding energy of -5.07 kcal/mol and inhibition constant of 192.57µM.
Conclusion: The results of our investigation suggested that garlic phytochemicals can have a good impact against black fungi, pertaining to the significant binding energies of phytoconstituents during blind docking. Specifically, Z-ajoene could be a good alternate against black fungi. However, detailed research is required to explore the antifungal activity of garlic against mucormycosi
0 notes
Text
Black Fungus: All You Need To Know
Commonly referred to as the Black Fungus, Mucormycosis is a rare fungal disease that comes from a mold that grows on decaying and rotting organic matter. Mucormycetes is the fungal mold that causes the infection and when a person is exposed to this, it affects the sinus and the eye region. The infection mainly affects those whose immune system is already weak or are under medication. The infection spreads when the body is not strong enough to fight the illness on its own.
0 notes
Text
The recent uptick in cases of the rare but deadly fungal infection, mucormycosis, in COVID-19 patients has shone a spotlight on the need for better prevention and treatment options. Mucormycosis, also known as black fungus, can lead to serious illnes...
#Mirari #MirariDoctor #MirariColdPlasma #ColdPlasma
0 notes