#imagenology
Text

I have a tree in my head and no one told me...
#science#neurology#neuroscience#imagenology#tractografia#physiotherapy#physiology#human body#human mind
1 note
·
View note
Photo

☢️El síndrome o fenómeno de Lázaro. ( EL REGRESO. DE LA MUERTE. )☢️ Se refiere a la recuperación de algunos signos vitales después de que se ha determinado la muerte del paciente: frecuencia cardiaca, automatismo respiratorio, restauración de la circulación e incluso movimiento de grupos musculares; generalmente, este fenómeno ocurre entre los 10 y 15 minutos, y es aun más probable que se presente después de que el paciente ha recibido maniobras de resucitación cardiopulmonar, aunque también se han reportado casos en donde se presenta después de abusar de drogas consideradas como recreativas . ☢️Aun cuando los casos reportados con este fenómeno son afortunadamente pocos, el síndrome de Lázaro plantea cuestiones legales y éticas en el médico encargado de determinar el momento de la muerte de un paciente, así como el momento en que deben suspenderse las maniobras de reanimación, o bien proceder a estudios o procedimientos post mortem como la autopsia o la donación de órganos. #ultrasound #ultrasounds #radiology #radiología #ultrasonido #imagenology #imagenología #medicina #medicinahumana #docescalona #med #instadoc #doctor #medicinalegal #estudiantemedicina #medicine #instadoctor #rx #ecografía #ecography #eco #usd #sonograph #sonographer #muerte #sindrome #gris #dark #oscuro (en Isla de Margarita- Tu Destino Ideal) https://www.instagram.com/p/CSlRNxsNOZT/?utm_medium=tumblr
#ultrasound#ultrasounds#radiology#radiología#ultrasonido#imagenology#imagenología#medicina#medicinahumana#docescalona#med#instadoc#doctor#medicinalegal#estudiantemedicina#medicine#instadoctor#rx#ecografía#ecography#eco#usd#sonograph#sonographer#muerte#sindrome#gris#dark#oscuro
0 notes
Photo

Title: Deviation of the Spine Study 7 Artist: Veronica Huacuja Medium: Oil, acrylic on paper Size: 9 (W) x 12 (H) x 0.1 in Year: 2018 Just like some paints exhibit a flying bird among the white clouds, this artwork exposes–with all its drama–a "human landscape", which is an inner sight of a congenital illness that deforms the body. The initial sources of this artwork are diverse X-rays medical studies done to an anonymous person. Thank you for reading. #scoliosis, #art, #artist, #deviationofthespine, #xray, #radiology, #paint, #painting, #artpal, #neug, #artwebsite; #stippling; #painter; #oil; #acrylic, #artist; #oilpainting; #patreon, #expressionism, #mexicancontemporaryart, #mexicancontemporaryartist, #gesso, #fabriano, #italianpaper, #imagenology, #expressionismart, #expressionisminfigurative, #oilonpaper, #x-ray, #x-rays, #singulart, #artpal, #neug https://www.instagram.com/p/CHYkPIrHZJw/?igshid=vyrcd2kjq0kr
#scoliosis#art#artist#deviationofthespine#xray#radiology#paint#painting#artpal#neug#artwebsite#stippling#painter#oil#acrylic#oilpainting#patreon#expressionism#mexicancontemporaryart#mexicancontemporaryartist#gesso#fabriano#italianpaper#imagenology#expressionismart#expressionisminfigurative#oilonpaper#x#singulart
16 notes
·
View notes
Text
This is gonna be my shifting journal mostly, I’m a baby shifter I started not too long ago, keep in mind I am also a medicine student and I’m doing a minor career at the same time for medical imagenology this is for me mostly, and to keep track of my development so you’re free to take a look!
2 notes
·
View notes
Note
12 for Takari?
OOOH GOD, I really had issues over how to write this one, but I finally managed to do it.
I think it turned out pretty well all things considered :). I really hope you like it.
Send me ask & MasterPost
I am pregnant
“She used to say that the human heartbeat was the first music that a person heard, and that every child was born knowing the rhythm of her mother's song.”
― Kate Morton
She’d been feeling sluggish lately. It was nothing out of the ordinary and she blamed it to work since she’d been having some rough days recently. She should have seen it coming when she enlisted to help out at the ER onJou’s request. The Koushiro Incident was the cherry on top of the day. Jou had decided to save his opinions out of consideration for his old friend, but she had caught him trying to keep himself from laughing several times after the whole incident was over.
Who would have imagined that coconut oil could cause so much trouble?
Yamato and Taichi had been way too drunk to remember most of the incident, but Takeru who had been the chaperone during the bachelor party had witnessed everything and she had caught him writing something in his notebook at the hospital cafeteria later that night. He hadn’t told her what it was, but she was slightly suspicious that her dear husband was actually recounting the whole incident to use a funny story to retell in the future. Fortunately, Koushiro’s little problem had been solved with some epinephrine and steroids and they hadn’t had to lament any losses.
Still Hikari didn’t remember ever feeling this off, not even during her internship time, and those days had been the most tiring of all
“You’re not looking too hot,Yagami. You okay?” Yoshinori-san, the head nurse of the ER said.
“Yeah...I’m feeling a little tired.”
“Tired? Well, yeah. It’s been busy lately, isn’t it?” Yoshinori-san said with a nod “But you should talk to doctor Kido. There seems to be a cold bug going around. I’ve seen a lot of people with cold symptoms coming in.”
“Yes, I don’t think it is a cold. I don’t feel feverish…” Hikari said, feeling her forehead “but I will ask Jou-senpai to be sure. Thank you, Yoshinori-san.”
Jou was sitting in his office with a face that did not hide his exhaustion; he rested his head over the desk wondering if he could spare a couple minutes of sleep when he heard a timid knock on his door. Hikari was standing in front of the door with the same tired look that he had, holding two steaming cups in his hands.
“Oh..hey…” Jou said, fixing his glasses back in place.
“Hey, long night, huh? I brought you something and I know, I asked for soy milk...don’t worry.” she added when Jou was about to comment. Her childhood friend smiled and accepted the cup, enjoying the comforting warmth between his fingers.
“Long... That’s an understatement…” Jou coughed “Never had I imagined I’d have to attend one of my friends in such...curious condition.”
Hikari giggled.
“And even less that that friend would be Koushiro-san.”
“Yeah...I could have expected it from Taichi or Daisuke; hey even Yamato, but Koushiro?” Jou snorted, taking the cup to his lips. He had expected coffee, but to his surprise, it was tea.” Oh, not coffee today?”
“Uh...yeah, sorry. I intended to get you coffee, but the smell just made me feel sick.”
That couldn’t be right, Jou thought. He put down the cup and looked at the woman sitting in front of him with an inquisitive look. He had known her for almost all his life, and he was well aware of her fragile health. Though it had improved considerably in the last few years, worrying and sounding an alarm at the slightest hint that she wasn’t feeling alright had become a habit of his.
“Sick?”
“Yeah, I haven’t been feeling too well lately” she said casually. Hikari leaned on the desk and began pressing her temple. A mild headache was starting to hit her, and it was making her feel a little dizzy and lightheaded “I guess it might be fatigue. I mean, I’ve been so tired lately.”
“Well, the ER is a busy department…” Jou admitted “but still, when it comes to you...sometimes it is better to be safe.”
She somehow knew that he’d said that. Well, she’d come ready to receive an impromptu health examination from the start, so she didn’t complain.
“So...nausea?” Jou asked.
“Yeah, pretty often lately and very sporadic.Strong smells make it worse.”
“Fever? Coughing?”
“No, normal temperature, I think?” she shrugged “I mean it's mostly fatigue, nausea, dizziness and mild headaches…”
Jou was writing down the symptoms in a notepad, when a sudden thought hit him.
“Hikari-chan...when was your last period?”
Jou and Hikari looked at each other for a moment. SInce both of them had been working together regularly and were very professional, their expressions were serene.However, it didn’t make the silence less awkward.
“Eh...last month?” Hikari said, unsure “I can’t remember. I think I am a little late this month, but I’ve never been regular so…”
“Well, in your situation...I wouldn’t scratch the possibility. Let’s run a test, just to be sure shall we?”
The hCG test results arrived faster than Hikari had expected and Hikari suspected that Jou might have used his influences in the lab. Her friend entered the office with a stoic expression.
“So?” Hikari asked expectantly.
“Eh, yeah...I think we need to make a quick stop at imagenology, Hikari-chan.”
Hikari was speechless and for a brief moment considered pinching herself to make sure she hadn't fallen asleep in the nurses' room and was dreaming.
Jou smiled and handed her the lab result. Written in small letters said Positive and next to the result was a scribble that Hikari recognized as Jou's handwriting: "Congratulations, you're going to be a mom!"
The events that followed this revelation were like a blur: Jo accompanied her to the imaging department, and the day's surprises (including Koushiro's unexpected visit to the ER) weren't ending.
Hikari was not only 11 weeks pregnant, but there were two small creatures growing in her womb and they both looked perfectly healthy. The girl could not contain her tears when she heard the small and rapid heartbeats of the two little ones.
“Well, look at that…” Jou grinned, as they walked back to the ER “Two little ones, huh? I can’t imagine Takeru’s face when you tell him.”
“Nor can I…” Hikari giggled, looking at the photo she was holding. A photo of her two babies.
“I can’t imagine Yamato nor Taichi’s faces either…” Jou laughed “Especially Taichi’s. I think he’s still in denial about the fact that you’re married and what that implies…”
Hikari laughed. Taichi was going to lose it and poor Takeru would be the victim, but maybe Yamato would give him a hand. She knew that once the shock had passed, Taichi would be overjoyed by the news.
“So how are you planning to tell him?”
“I think I might have an idea…”
It was later that day, when her shift ended that she snuck into Takeru’s study and scanned the ultrasound into his laptop and set it up as his desktop image with a tiny little sticky memo with one single sentence:Look at what we made.
She was in the kitchen when she heard the chair fall down, and patamon screeching desperately asking if his partner was ok? She simply smiled and rested her hand over her abdomen.
From all the surprises she got that day, this was definitely the best one yet.
=========================================================
As usual Here’s a chibi (sorry I can’t draw ultrasounds :P)
#Takari#forever#hikari yagami#kari kamiya#Digimon#fanfiction#AU#jou kido#jyou kido#Baby on the way#Digimon 2020#my drabbles#ugly chibi#Prompt challenge
39 notes
·
View notes
Text
Biomed Grid | Epidemiological Characteristics and Management of Brain Metastases on Patients in the Clinical Hospital of the University of Chile (Hcuch) between 2012 and 2017
Abstract
Introduction and Context: Brain metastases (BM) are the main neurological complication of cancer, affecting up to 30% of these patients (incidence = 8.3-14.3 x 100,000), and they are the most frequent intracranial tumors (IT) of the adult. They are 10 times more common than primary cerebral neoplasms (PCN), however, the number of publications about this pathology is only 25% of PCNs such as gliomas. In our country there is no national registry of brain tumors, so the actual incidence of these is unknown. Treatments include initial/palliative management with glucocorticoids (GC) and/or surgery (Cx), radiosurgery (RS) or Whole Brain Radiation Therapy (WBRT). The purpose of this study is to determine clinical and therapeutic characteristics of BM in patients taken care of in our institution and with this information we propose the improvement of the management of these patients.
Material and Methods: In this cohort study we analyze the clinical records of patients treated in our hospital during the years 2012-2017 with a diagnosis of BM. The date of death was obtained from the National Identification Registry and Identification Service and calculated the median survival between diagnosis and death. We registered: sex, age at diagnosis, number of brain metastases, management and survival rate.
Results: 54 CR were found with a diagnosis of BM, however, only 31 complied with Inclusion criteria (IC). Average age at diagnosis of symptomatic BM: 59 years (range: 29-86 years), men (n=13): 56.3 years and in women (n=18): 60.9 years. BM number: 14 patients (45,1%) had one BM; 11 (35,5%) had oligometastases (2 or 3); and 6 (19,4%) patients multiple BM (more than 3). Origin of primary tumor: 45.2% pulmonary; 12.9% colorectal; 12.9% renal; 9.7% breast; 3.2% ovary; 3.2% unknown; 12.9% other (Includes gastric, hepatic and thyroid). Only 38.7% of BM had BB, 25% were poorly differentiated lung carcinoma, 16.7% colon adenocarcinoma and 16.7% moderate/poorly differentiated breast carcinoma. Clinical Features (CF) highlights includes motor symptoms and signs in 54,8%, headache in 48,4% and gait apraxia in 38,7%. Location: 67.7% of patients had hemispheric tumors and 35.5% cerebellar. There were no brainstem tumors in our study. 12 (38.7%) patient received active treatment (surgery or radiosurgery),11 (35.5%) had surgery and only one (3.2%) received radiosurgery. All patients received palliative care, and 10 received WBRT. Survival: one patient was alive. For those who had a certified death, average survival time after diagnosis was 34.9 weeks (N=30). People who received active treatment, had an average survival time of 56.1 weeks after diagnosis and 54.5 weeks after treatment (N=12). Patients which did not receive an active treatment (N=18) had an average survival of 20.7 weeks. The hazard rates differ between those who had an active treatment and those who did not (log-rank test), z test = 2.25, p = 0.0246).The survival -in weeks- of patients who WBRT (N=10) versus those that were only managed with palliative care (GC) (N=8) was z test = 2.76, p = 0.00578. In the group of people who received active treatment, there was no difference between the ones that had unique BM vs those with 2 or 3 BM. In the group that received active treatment, 3(25%) patients died because of their BM but there was no difference with the palliative group.
Conclusion: BM is a prevalent oncological complication. The age of presentation is primarily between 4th-7th decade of life, the main primary tumor comes from lung, and the main location is at the frontal lobe. All patients should be given palliative treatment and active treatments are offered to selected patients with better prognosis. The average survival for patients with active treatment in our institution is 54.5 weeks better than the WBRT and palliative group.
Keywords: Cancer; Brain metastases; Brain radiotherapy; Palliative care
Abbreviations: PCN: Primary Cerebral Neoplasms; BM: Brain Metastases; IT: Intracranial Tumors; CNS: Central Nervous System; CF: Clinical Features; GC: Glucocorticoids; SRS: Stereotactic Radiosurgery; WBRT: Whole Brain Radiation Therapy; CR: Clinical Records; IC: Inclusion Criteria; BB: Brain Biopsies; EC: Exclusion Criteria
Introduction
Brain metastases (BM) is the main direct neurological complication of cancer and the most frequent intracranial tumors (IT) in adults [1]. They are ten times more frequent than primary cerebral neoplasms (PCN) and its current management involves mostly palliative therapy but is at this moment evolving towards an active therapy either by surgical means or radiosurgery, which has shown a better prognosis [2]. The number of published papers on BM only achieves 25% of gliomas [3]. Metastases to Central Nervous System (CNS) are common, affect 30% of patients with cancer [4]. BM are the most frequent expression of intracranial malignancy with an incidence varying between 8.3 and 14.3 per 100,000 [5]. However, are not the intracranial tumors most frequently operated, it is estimated that around 20-25% of BMs have a surgical indication. The candidates for surgery are patients with best prognostic factors, such as: age, controlled systemic disease, good functional status (Karnofsky), usually single and localized in non-eloquent area. The cause of death of these patients is in most cases due to metastatic disease and only 25% die of neurological causes [6]. In our country there is no national registry of brain tumors, so the actual incidence of these is unknown [7]. 80% of CNS metastases are in the hemispheres, particularly in the territory of the middle cerebral artery and the posterior cerebral artery. In descending order: frontal, parietal, temporal and occipital [8]. The origin of BM highlights lung cancer, following with lower percentages breast cancer and melanoma [9]. BM are more frequent between the fifth and seventh decade of life and 75% of patients have multiple metastatic tumors [10]. The clinical features (CF) are varied, including headache as an initial symptom in 50% of patients [11]. Treatments include: initial/palliative management with glucocorticoids (GC) and/or surgery (Cx), stereotactic radiosurgery (SRS) or Whole Brain Radiation Therapy (WBRT) [6].
Objective
To study and describe epidemiological and clinical-therapeutic characteristics of BM patients in the Clinical Hospital of the University of Chile (HCUCH).
Methodology
This is a cohort study of a cross-section period between 2012 and 2017. The information was obtained from clinical records (CR) of patients treated at the HCUCH. Inclusion criteria (IC) and exclusion criteria (EC) were defined based on the available clinical records:
IC: adult patients diagnosed with BM during 2012-2017.
EC: incomplete registry and/or diagnostic doubt between primary brain neoplasm and BM.
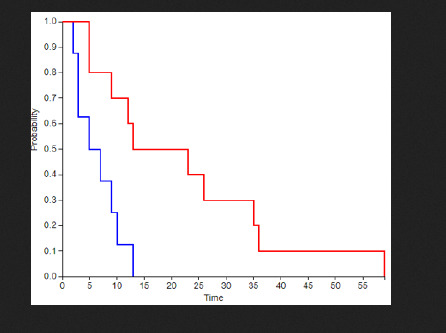
The following data was registered: sex, age at diagnosis, BM number, clinical features, primary cancer, clinical status, management and outcome. We also reviewed reports of pathological anatomy of existing brain biopsies (BB) of patients who met the IC. The cause and date of death was obtained from the death certificates of the National Identification Registry and CR. Survival was estimated from the date of imagenologic diagnosis to the date of death for all patients. Subsequently, the information was analyzed, and the Kaplan-Meier survival curves were configured using the Log-Rank Test, comparing survival rates between active vs non-active treatment. Significance was established when p < 0.05. This report was approved by the ethics committee from HCUCH.
Results
54 CR were found with a diagnosis of BM, however, only 31 complied with IC (Graph 1). Average age at diagnosis of symptomatic BM: 59 years (range: 29-86 years), men (n=13): 56.3 years and in women (n=18): 60.9 years (Graph 2). BM number (Graph 3): 14 patients (45,1%) had one BM; 11 (35,5%) had oligometastases (2 or 3); and 6 (19,4%) patients multiple BM (more than 3). Origin of primary tumor: 45.2% pulmonary; 12.9% colorectal; 12.9% renal; 9.7% breast; 3.2% ovary; 3.2% unknown; 12.9% other (Includes gastric, hepatic and thyroid) (Graph 4). Only 38.7% of BM had BB, 25% were poorly differentiated lung carcinoma, 16.7% colon adenocarcinoma and 16.7% moderate/poorly differentiated breast carcinoma (Graph 5). Clinical Features (CF) highlights includes motor symptoms and signs in 54,8%, headache in 48,4% and gait apraxia in 38,7% (Table 1). Location: 67.7% of patients had hemispheric tumors and 35.5% cerebellar (Figure 1). There were no brainstem tumors in our study. 12 (38.7%) patients received active treatment (surgery or radiosurgery),11 (35.5%) had surgery: tumor resection including one ventricular peritoneal shunt and only one (3.2%) treated with radiosurgery. All patients received palliative care, and 10 received WBRT.
Graph 1: Case records of patients with cerebral metastases attended between 2012 and 2017 at HCUCH (N=31).
Graph 2:Age distribution (N=31).
Graph 3: Number of BM per patient.
Graph 4: Histology of brain biopsies (N=12).
Graph 5: Survival curve between the group of death patients that were candidate to active management (red line n=12) versus those that were managed with palliative care (blue line n=18). Time expressed in weeks (N=30). z = 2.25, p = 0.0246.
Table 1: Frequency of symptoms and signs at clinical onset.
Note: *Cognitive impairment was found only in the group >50 years. may be because of there were only three frontal BM with mild simptoms. **Gait apraxia may be by less posterior fosa oligometastases.
Figure 1: Distribution of BM by location (N=69 tumors).
Survival: One patient is still alive. For those who had a certified death, average survival time after diagnosis was 34.9 weeks (N=30). People who received active treatment, had an average survival time of 56.1 weeks after diagnosis and 54.5 weeks after treatment (N=12). Patients which did not receive an active treatment (N=18) had an average survival of 20.7 weeks. The hazard rates differ between those who had an active treatment and those who did not (log-rank test), z test = 2.25, p = 0.0246).The survival in weeks of patients who WBRT (N=10) versus those that were only managed with palliative care (GC) (N=8) was z test = 2.76, p = 0.00578 (Graph 6). In the group of people who received active treatment, there was no difference between the ones that had unique BM vs those with 2 or 3 BM (Graph 7). Cause of death: In the group that received active treatment, 3 (25%) patients died because of their BM but there was no difference with the palliative grow. Future Proposals: Improvements to this project could include a multicentric analysis and a more thorough.
Graph 6: Survival curve between the group of death patients that were candidate to active management (red line n=12) versus those that were managed with palliative care (blue line n=18). Time expressed in weeks (N=30). z = 2.25, p = 0.0246.
Graph 7:Survival curve between the group of death patients that were candidate to active management with unique metastases (red line n=8) versus those with active management and oligometastases (blue line n=4). Time expressed in weeks (N=12). z = 0.27, p = 0.79.
Discussion
There are few Chilean studies about BM [2,12] In this study the age of presentation is mainly between 50 and 70 years (59.4%), including an important group of patients who were reported in their 4th decade of life (22.6%). Also 45.1% of patients had a single BM, 35.5% oligometastases and 19.4% of patients emerged with multiple BM, incidence that has not been reported as in other studies [10]. According to previous reports the leading origin of primary tumor was pulmonary (45.2%), but our breast incidence (9.7%) was lower than other reports and colorectal and renal (12.9%) were higher. None of our patients was reported with melanoma. A major group displayed hemispheric tumors (frontal, parietal, occipital, temporal) followed by a significant pool of cerebellar tumors, as in other papers [10]. The clinical presentation coincides with the literature including headache in nearly 50% of patients, and an important group with motor symptoms and signs (54.8%) and gait apraxia (38.7%). Cognitive impairment was found only in the group >50 years. may be because of there were only three frontal BM with mild symptoms and also gait ataxia was not found because of less posterior fossa oligometastases.
According with other studies [13] 25% of our patients with active treatment died because of neurological associated causes. It is important to consider that only patients in good functional status and with a small number and size of BM were candidates to active treatment. There was a significant difference in survival between patients who received active treatment and the group treated with palliative management (p<0.05). This result supports the active management in selected patients [12,14]. In our country radiosurgery is not available for all patients that is the reason for only one patient treated. There was also a significant difference when we compared WBRT versus palliative management. This has been reported in the literature since several years [15].
Conclusion
Brain Metastases are an important oncologic complication. As in other studies, we found that the average age of presentation is in between the fourth and seventh decade of life, also that pulmonary cancer is the main primary on these patients and the main location for these metastases is the frontal lobe. Palliative care is mandatory for all these patients, but active management must be given to selected patients with a better prognosis. All patients should be discussed in the neuro-oncological committee to evaluate the possibility for an active treatment such as surgical or radio surgical treatment. Future Proposals: Improvements to this project could include a multicentric analysis.
Read More About this Article: https://biomedgrid.com/fulltext/volume2/epidemiological-characteristics-and-management-of-brain-metastases-on-patients.000608.php
For more about: Journals on Biomedical Science :Biomed Grid
#biomedgrid#List of open access medical journal#Journals on medical research#medical and medicinal journal#Open access clinical and medical journal#Journals on Biomedical Engineering
0 notes
Text
UASLP, inicio Encuentro de Imagenología y reconoce labor del Dr. Daniel Silva-Herzog Flores
https://acontecersanluis.wixsite.com/acontecersanluis/single-post/2019/02/08/UASLP-inicio-Encuentro-de-Imagenolog%25C3%25ADa-y-reconoce-labor-del-Dr-Daniel-SilvaHerzog-Flores
View On WordPress
0 notes
Text
¡Descarga TikTok para compartir $ 35 conmigo! Únete hoy para ganar recompensas en efectivo. https://vm.tiktok.com/ZSVF7t56/
1 note
·
View note
Photo

Soy una persona valiosa e imprescindible. ✨ #worldofxray #radiology #imagenology #xray #resonance #irm #rmn #magnetic https://www.instagram.com/p/BqLE2kdgY4m/?utm_source=ig_tumblr_share&igshid=4rx1fhmzyjf
1 note
·
View note
Photo

Paciente femenina 13 años de edad TC TÓRAX . . . . . . . . . . . . . . . . #ct #tc #tac #torax #spine #chest #anatomy #escoliosis #xray #tomography #worldofxray #radiology #imagenology #medicine #medschool #xrayschool https://www.instagram.com/p/BpoHShkAEJo/?utm_source=ig_tumblr_share&igshid=10rtiwr7r68yl
#ct#tc#tac#torax#spine#chest#anatomy#escoliosis#xray#tomography#worldofxray#radiology#imagenology#medicine#medschool#xrayschool
1 note
·
View note
Video
☢️Protrusion Prostática Intravesical☢️ Una excelente herramienta para el diagnóstico como predictor de la obstrucción de salida vesical y como vaticinador del resultado del retiro de Sonda. ☢️Se clasifica por grados☢️ Grado 1️⃣. <5 mm Grado 2️⃣. 5 - 10 mm Grado 3️⃣. > 10 mm P.D. No debe sustituir los scores de la uroflujometria, el volumen urinario residual o el volumen prostático. #ultrasound #ultrasounds #radiology #radiología #ultrasonido #imagenology #imagenología #medicina #medicinahumana #docescalona #med #instadoc #doctor #usmle #estudiantemedicina #medicine #instadoctor #rx #ecografía #ecography #eco #usd #sonograph #sonographer #prostata #urologia #urology #urologo (en Isla de Margarita- Tu Destino Ideal) https://www.instagram.com/p/CScB_FbHeU_/?utm_medium=tumblr
#ultrasound#ultrasounds#radiology#radiología#ultrasonido#imagenology#imagenología#medicina#medicinahumana#docescalona#med#instadoc#doctor#usmle#estudiantemedicina#medicine#instadoctor#rx#ecografía#ecography#eco#usd#sonograph#sonographer#prostata#urologia#urology#urologo
0 notes
Photo

☢️Vitiligo☢️ ☢️El vitíligo es una enfermedad que causa la pérdida de color de la piel en manchas. Las áreas descoloridas generalmente se agrandan con el tiempo. La afección puede afectar a la piel de cualquier parte del cuerpo. También puede afectar al cabello y al interior de la boca. ☢️Normalmente, el color del cabello y la piel está determinado por la melanina. El vitíligo se produce cuando las células que producen melanina mueren o dejan de funcionar. Afecta a las personas de todo tipo de piel, pero puede ser más perceptible en las personas de piel más oscura. 👉Esta afección no pone en riesgo la vida ni es contagiosa👈. Puede ser estresante y hacerte sentir inseguro de ti mismo. ☢️El tratamiento para el vitíligo puede restaurar el color de la piel afectada. Pero no previene la continua pérdida de color de la piel o una recurrencia. ☢️Es difícil predecir cómo progresará la enfermedad. A veces, las manchas dejan de formarse sin tratamiento. En la mayoría de los casos, la pérdida de pigmentación se extiende y con el tiempo afecta a la mayor parte del cuerpo. Ocasionalmente, la piel recupera su color. ☢️Causas Un trastorno del sistema inmunitario (afección autoinmunitaria) Antecedentes familiares (herencia) Un evento desencadenante, como el estrés, una quemadura por el sol grave o un traumatismo en la piel, como el contacto con una sustancia química ☢️Diagnóstico☢️ El médico probablemente te preguntará sobre tus antecedentes médicos y te examinará la piel, posiblemente con una lámpara especial. Tu evaluación también puede incluir una biopsia de piel y análisis de sangre. ☢️Tratamiento☢️ La elección del tratamiento depende de la edad, la extensión y la ubicación de la piel involucrada, la velocidad de avance de la enfermedad y de cómo afecta tu vida diaria #ultrasound #ultrasounds #radiology #radiología #ultrasonido #imagenology #imagenología #medicina #medicinahumana #docescalona #med #instadoc #doctor #usmle #estudiantemedicina#medicine #instadoctor #rx #ecografía #ecography #eco #usd #sonograph #sonographer (en Isla de Margarita- Tu Destino Ideal) https://www.instagram.com/p/CRr5KBtFyny/?utm_medium=tumblr
#ultrasound#ultrasounds#radiology#radiología#ultrasonido#imagenology#imagenología#medicina#medicinahumana#docescalona#med#instadoc#doctor#usmle#estudiantemedicina#medicine#instadoctor#rx#ecografía#ecography#eco#usd#sonograph#sonographer
0 notes
Photo

☢️Avances en la investigación del cáncer de mama☢️ 🤔 ☢️Los investigadores financiados por el NCI están trabajando para mejorar nuestra comprensión de cómo prevenir, detectar y tratar el cáncer de mama. También están estudiando cómo abordar las disparidades y mejorar la calidad de vida de los sobrevivientes de la enfermedad. ☢️Una nueva tecnología es la mamografía 3D, también llamada tomosíntesis de mama. Este procedimiento toma imágenes desde diferentes ángulos alrededor del seno y las construye en una imagen similar a una 3D. Aunque esta tecnología está cada vez más disponible en las clínicas, no se sabe si es mejor que la mamografía 2D estándar para detectar el cáncer en una etapa menos avanzada, pero si logra un mejor desempeño en el reconocimiento de caracteres de muy alta fiabilidad para un diagnóstico. ☢️El NCI está financiando un ensayo de cribado mamario aleatorizado a gran escala, el Tomosynthesis Mammographic Imaging Screening Trial (TMIST), para comparar el número de cánceres avanzados detectados en mujeres examinadas durante 5 años con mamografía 3-D con el número detectado en mujeres examinadas con 2 -D mamografía. ☢️Dos preocupaciones en la detección del cáncer de mama, como en todas las pruebas de detección del cáncer, son la posibilidad de diagnosticar tumores que no amenacen la vida (sobrediagnóstico) y la posibilidad de recibir resultados falsos positivos. A medida que el tratamiento del cáncer se vuelve más individualizado, los investigadores están buscando formas de personalizar las pruebas de detección del cáncer de mama. Están estudiando métodos de detección que son apropiados para el nivel de riesgo de cada mujer y limitan la posibilidad de sobrediagnóstico. #ultrasound #ultrasounds #radiology #radiología #ultrasonido #imagenology #imagenología#medicina #mama #breastcancer #medicinahumana #docescalona #med #instadoc #doctor #usmle #estudiantemedicina #medicine #instadoctor #rx #ecografía #ecography #eco #usd #sonograph #sonographer #cancer #oncologia #oncology (en Isla de Margarita- Tu Destino Ideal) https://www.instagram.com/p/CRPa50LlmDW/?utm_medium=tumblr
#ultrasound#ultrasounds#radiology#radiología#ultrasonido#imagenology#imagenología#medicina#mama#breastcancer#medicinahumana#docescalona#med#instadoc#doctor#usmle#estudiantemedicina#medicine#instadoctor#rx#ecografía#ecography#eco#usd#sonograph#sonographer#cancer#oncologia#oncology
0 notes
Photo

☢Esta es la importancia de la vacunación☢ P.D Tomado del muro de Facebook de Dr. Yosmel Acosta Médico Internista Especialista en Nefrología y Cuidados Intesivos. #ultrasound #ultrasounds #radiology #radiología #ultrasonido #imagenology #imagenología #medicina #medicinahumana #docescalona #med #instadoc #doctor #usmle #estudiantemedicina #medicine #instadoctor #rx #ecografía #ecography #eco #usd #sonograph #sonographer #medicinainterna #medicointernista (en Isla de Margarita- Tu Destino Ideal) https://www.instagram.com/p/CQ8kgzYFeme/?utm_medium=tumblr
#ultrasound#ultrasounds#radiology#radiología#ultrasonido#imagenology#imagenología#medicina#medicinahumana#docescalona#med#instadoc#doctor#usmle#estudiantemedicina#medicine#instadoctor#rx#ecografía#ecography#eco#usd#sonograph#sonographer#medicinainterna#medicointernista
0 notes
Photo

☢Fascitis plantar☢ Implica la inflamación de una banda gruesa de tejido que atraviesa la planta del pie y conecta el hueso del talón con los dedos de los pies (fascia plantar). ☢Síntomas☢ Causa un dolor lacerante en la planta del pie cerca del talón. Por lo general, el dolor es más intenso al dar los primeros pasos después de despertarse, aunque también puede ser desencadenado por estar de pie durante mucho tiempo o al levantarse después de estar sentado. El dolor suele empeorar después del ejercicio, no durante este. ☢Diagnóstico☢ La fascitis plantar se diagnostica con base en los antecedentes médicos y el examen físico. Durante el examen, el médico revisará si hay áreas de sensibilidad en el pie. La ubicación del dolor puede ayudar a determinar su causa. ☢Estudios de diagnóstico por imágenes☢ Tu médico podría sugerirte una radiografía o una resonancia magnética o una ecografía de partes blandas región plantar para asegurarse de que otro problema, como una fractura por estrés, no te esté causando dolor. Algunas veces, una radiografía muestra un pedazo de hueso que sobresale (espolón) del hueso del talón. En el pasado, a menudo se creía que estos espolones óseos eran responsables del dolor en el talón y se extirpaban quirúrgicamente. Pero muchas personas que tienen espolones óseos en los talones no tienen dolor en el talón. ☢Tratamiento☢ La mayoría de las personas que tienen fascitis plantar se recupera en unos meses con un tratamiento conservador, que incluye reposo, aplicación de hielo en el área dolorosa y estiramiento. #ultrasound #ultrasounds #radiology #radiología #ultrasonido #imagenology #imagenología #medicina #medicinahumana #docescalona #ortopedia #traumatologia #fascitisplantar #instadoc #doctor #estudiantemedicina #medicine #instadoctor #rx #ecografía #ecography #eco #usd #sonograph #sonographer #islamargarita (en Isla de Margarita- Tu Destino Ideal) https://www.instagram.com/p/CQ1zQf-FnEd/?utm_medium=tumblr
#ultrasound#ultrasounds#radiology#radiología#ultrasonido#imagenology#imagenología#medicina#medicinahumana#docescalona#ortopedia#traumatologia#fascitisplantar#instadoc#doctor#estudiantemedicina#medicine#instadoctor#rx#ecografía#ecography#eco#usd#sonograph#sonographer#islamargarita
0 notes