#hypokalemia
Text
Hypokalaemia ECG changes
U have no pot and you have no T
but you have a long PR and a long QT
Low potassium causes:
U waves (small deflection immediately after T wave)
Flattened/inverted T waves
Prolonged PR interval
Apparent prolonged QT interval (due to fusion of T and U waves)
Also:
Increased P wave amplitude
Widespread ST depression
#medical school#med school#medicine#med student#medical student#medblr#medspo#revision#mnemonics#ecg#cardiology#hypokalaemia#hypokalemia#potassium#studyblr
11 notes
·
View notes
Text
When caring for a patient in cardiac arrest, it is important to recognize reversible causes for the arrest and address them. This is especially important with PEA and asystole, which often have reversible underlying causes. The mnemonic Hs and Ts can help you to remember the reversible causes of cardiac arrest.
Hypovolemia
Hypoxia
Hydrogen ion excess (acidosis)
Hyper- or hypokalemia
Hypothermia
Toxins
Tamponade
Tension pneumothorax
Thrombosis (pulmonary embolism)
Thrombosis (myocardial infarction)
In patients with metabolic acidosis, the administration of an initial dose of sodium bicarbonate (1 mEq/kg) may be indicated. If administering sodium bicarbonate, ensure adequate ventilation for removal of carbon dioxide or sodium bicarbonate may worsen intracellular and tissue acidosis.
Suspect hyperkalemia in all patients with acute or chronic renal failure and in those who had a wide-complex ventricular rhythm and tall, peaked T waves on ECG before arrest. Several measures may be taken to reduce potassium levels, including administering sodium bicarbonate, glucose and insulin, or nebulized albuterol. Sodium bicarbonate is preferred in patients with cardiac arrest caused by hyperkalemia because it causes a rapid shift in serum potassium level. Other therapies take much longer to work.
Suspect hypokalemia in patients with dehydration or overuse of diuretics. In hypokalemia, flat T waves, prominent U waves and possibly prolonged QT intervals may be seen on ECG before arrest. Treatment is with intravenous (IV) administration of a dilute solution of potassium chloride.
7 notes
·
View notes
Text

still here still kicking it
30 notes
·
View notes
Photo

🧠 HYPOKALEMIA Dose of i.v Potassium Chloride KCL MedNote Collection --------------------------------- instagram.com/mednotecollection t.me/MedNoteCollection pinterest.com/MedNoteCollection fb.me/MedNoteCollection --------------------------------- #medicine #medical_student #doctor #mednote_collection #MedNoteCollection #usmle #mrcp #pharmacology #pharma #Hypokalemia #endocrinology #ICU https://www.instagram.com/p/Cqv0gPZM7kr/?igshid=NGJjMDIxMWI=
#medicine#medical_student#doctor#mednote_collection#mednotecollection#usmle#mrcp#pharmacology#pharma#hypokalemia#endocrinology#icu
0 notes
Text
Lack of potassium: symptoms of hypokalemia
Lack of potassium: symptoms of hypokalemia
Published on 25/12/2022 at 7:22 p.m.
Updated 25/12/2022 at 7:22 p.m.
in collaboration with
Sarah Rebert (emergency physician)
What does potassium do in our body? What are the symptoms of a potassium deficiency? What are the causes ? How to diagnose and treat it? The point with doctor Sarah Reber, emergency doctor.
What is the interest of potassium?
“Like sodium, potassium is an electrolyte…

View On WordPress
1 note
·
View note
Text
Is your body lacking enough Potassium?
Is your body lacking enough Potassium?
Our body needs electrolytes (minerals) that carry an electric charge when they’re dissolved in bodily fluids and perform various functions. Potassium is one such electrolyte that our body needs for cells, muscles and nerves to function properly and as a natural process our kidneys remove excess potassium through urine to keep a proper balance of the mineral in the body.
What causes Low Potassium…
View On WordPress
#Benefits of potassium#Causes of low potassium in body#Foods rich in potassium#Foods sources of potassium#Hypokalemia#Low potassium#Muscle cramping#Symptoms of low potassium
0 notes
Text
Legs working now, but weekend gone. On the plus side, I have eaten a sum total of 25 bananas, and I think that's impressive. 🍌🍌🍌🍌🍌🍌🍌🍌🍌🍌🍌🍌🍌🍌🍌🍌🍌🍌🍌🍌🍌🍌🍌🍌🍌
1 note
·
View note
Text
Top 10 Potassium Rich Foods
1. Dry Fruits
2. Avocado
3. Bananas
4. Coconut Water
5.Potatoes
6. Tomato
7. Salmon
8. Yogurt
9. Spinach
10.Cucumber
#patients#Best foods#healthy foods#Potassium rich foods#foods for hypokalemia patients#potassium rich diets
0 notes
Text
Here's a list of common signs and symptoms associated with the deficiency of each electrolyte:
Low Sodium (Hyponatremia):
Headache
Nausea and vomiting
Fatigue and weakness
Confusion or altered mental state
Seizures
Muscle cramps or spasms
Swollen hands and feet (edema)
Low blood pressure
Rapid heart rate
Low Potassium (Hypokalemia):
Muscle weakness or cramps
Fatigue
Constipation
Irregular heart rhythm (arrhythmia)
Tingling or numbness
Weakness or paralysis (in severe cases)
Increased thirst
Abdominal cramping or bloating
Low blood pressure
Low Calcium (Hypocalcemia):
Muscle cramps or spasms
Numbness or tingling in hands, feet, or face
Weak or brittle nails
Tooth decay
Osteoporosis (bone loss)
Tetany (muscle twitching or spasms)
Confusion or memory problems
Depression or irritability
Abnormal heart rhythms
Low Magnesium (Hypomagnesemia):
Muscle cramps or twitches
Tremors or shaking
Muscle weakness
Fatigue
Irregular heartbeat
Nausea and vomiting
Loss of appetite
Personality changes
Seizures (in severe cases)
Low Chloride (Hypochloremia):
Muscle weakness
Excessive sweating
Irregular heart rhythms
Dehydration
Confusion or changes in mental status
Nausea and vomiting
Diarrhea
Hyperventilation (rapid breathing)
Low Bicarbonate (Hypobicarbonatemia):
Deep and rapid breathing
Confusion or disorientation
Weakness or fatigue
Dizziness or lightheadedness
Nausea and vomiting
Headache
Coma (in severe cases)
Low Phosphate (Hypophosphatemia):
Muscle weakness
Fatigue
Bone pain or tenderness
Difficulty breathing
Loss of appetite
Irritability
Confusion or altered mental status
Abnormal heart rhythms
Signs and symptoms of low electrolytes can vary depending on which specific electrolyte is deficient. If you suspect an electrolyte imbalance, it's essential to seek medical evaluation and diagnosis to determine the underlying cause and receive appropriate treatment.
#ed not ed sheeran#ed not sheeren#ed no sheeran#disordered eating thoughts#tw ana shit#tw ed diet#ed bllog#anorex14#ana trigger#ana shit#tw ana diary#4norexi4#thin$spo#thinspø#th!n$spo#⭐ving#⭐ve#tw ed rant#ed vent#xseffortpost
2K notes
·
View notes
Text
I'm covering for a pt who has hypokalemia to 2.9. The nurse notified me, so I got a stat EKG. The EKG showed normal sinus rhythm. I don't know the pt's cardiac hx (e.g., heart failure), so I don't want to give her too much fluid, but she is NPO, so she has to get the potassium IV. I ordered potassium chloride, 20 mEq in 50 mL NS to be infused at a rate of 25 mLs/hour x4 bags. The nurse then asked me if I wanted to infuse at a faster rate because it would take 2 hours for each bag to be infused. I know potassium hurts to receive as an IV. The recommendation is actually 20 mEq every 2 to 3 hours. You can only give 10 mEq/hr IV. If you want higher than 10 mEq, you have to use central line (the PA told me this). You should also check the magnesium level because if magnesium is low, that affects the potassium. If you give potassium to someone with low magnesium, the potassium repletion might not be effective. This is from UpToDate (skip to 9th paragraph):
Etiology – The most common causes of hypokalemia are gastrointestinal or urinary losses due to vomiting, diarrhea, or diuretic therapy. Hypokalemia may also result from the transient entry of potassium into cells, which is called redistributive hypokalemia.
●Clinical manifestations – Manifestations of hypokalemia include severe muscle weakness, cardiac arrhythmias, kidney abnormalities, and glucose intolerance. These signs and symptoms are generally proportionate to the degree and rapidity of the reduction in serum potassium and resolve with correction of the hypokalemia. The risk of arrhythmias from hypokalemia is highest in older patients, patients with organic heart disease, and patients on digoxin or antiarrhythmic drugs.
●Management – The underlying cause of the hypokalemia should be identified, particularly the presence of hypomagnesemia or redistributive hypokalemia. Patients with hypomagnesemia can be refractory to potassium replacement alone, and potassium replacement can result in rebound hyperkalemia in patients with redistributive hypokalemia. Among patients with redistributive hypokalemia due to increased sympathetic tone (as in hypokalemic thyrotoxic periodic paralysis), the administration of a nonselective beta blocker, such as propranolol, can rapidly reverse the hypokalemia and associated symptoms.
•Mild to moderate hypokalemia – For patients with mild to moderate hypokalemia (serum potassium 3.0 to 3.4 mEq/L) who do not have ongoing urinary potassium losses, we suggest initial oral administration of 10 to 20 mEq of potassium given two to four times per day (20 to 80 mEq/day) (Grade 2B).
Oral potassium preparations include potassium chloride, potassium bicarbonate or its precursors (potassium citrate, potassium acetate), and potassium phosphate. Potassium chloride can be given in crystalline form (salt substitutes), as a liquid, or in a slow-release tablet or capsule. Potassium bicarbonate or its precursors are preferred in patients with hypokalemia and metabolic acidosis. Potassium phosphate should be considered only in patients with hypokalemia and hypophosphatemia, as might occur with proximal (type 2) renal tubular acidosis associated with Fanconi syndrome and phosphate wasting.
In patients who have chronic, stable renal potassium wasting, a potassium-sparing diuretic, such as amiloride, may be required should potassium repletion not be successful. (See 'Ongoing losses and the steady state' above and "General principles of disorders of water balance (hyponatremia and hypernatremia) and sodium balance (hypovolemia and edema)", section on 'The steady state'.)
Patients with primary aldosteronism also present with hypokalemia due to renal potassium wasting: Spironolactone or eplerenone is preferred for patients diagnosed with this disorder.
If a potassium-sparing diuretic is used in combination with potassium supplements, we recommend close monitoring of potassium levels, along with dietary assessment and limitation of dietary potassium intake. This combination must be used with extreme caution in patients with decreased kidney function and in patients on an ACE inhibitor, renin inhibitor, and/or angiotensin receptor blocker. We suggest monitoring the serum potassium concentration approximately every three to four months in all patients receiving chronic potassium supplementation, or more often if clinically indicated.
•Severe hypokalemia – Careful monitoring of the physiologic effects of severe hypokalemia (ECG abnormalities, muscle weakness, paralysis) is essential. Continuous ECG monitoring or telemetry is warranted in patients with arrhythmias caused by hypokalemia, prolonged QT and/or other ECG abnormalities attributable to hypokalemia, underlying cardiac issues that predispose to arrhythmia in the setting of hypokalemia (eg, digoxin toxicity, myocardial infarction, underlying long QT syndrome), and also when intravenous potassium repletion is given at a rate greater than 10 mEq per hour, or if patients are at risk for rebound hyperkalemia (most often due to thyrotoxic periodic paralysis).
Potassium must be given more rapidly to patients with hypokalemia that is severe (serum potassium less than 2.5 to 3.0 mEq/L) or symptomatic (arrhythmias, marked muscle weakness, or rhabdomyolysis). In such patients, potassium chloride can be given orally in doses of 40 mEq, three to four times per day or, particularly in patients also treated with intravenous potassium, 20 mEq every two to three hours. Careful monitoring of the serum potassium is also essential. We suggest that the serum potassium should initially be measured every two to four hours to ascertain the response to therapy. If tolerated, this regimen should be continued until the serum potassium concentration is persistently above 3.0 to 3.5 mEq/L and symptoms or signs attributable to hypokalemia have resolved.
For patients with severe manifestations of hypokalemia or those who are unable to take oral medications, we recommend intravenous potassium chloride (Grade 1B).
Depending upon the severity of symptoms, intravenous potassium may be given at doses ranging from 20 mEq every two to three hours to a recommended maximum rate of potassium administration of 10 to 20 mEq/hour for most patients; rates as high as 40 mEq/hour have been used for life-threatening hypokalemia. Rates above 20 mEq/hour are highly irritating to peripheral veins. When such high rates are given, they should be infused into a large central vein or into multiple peripheral veins.
In addition, the maximum amount of potassium that is added to each particular sized infusion container should be limited in order to decrease the risk of inadvertent administration of a large absolute amount of potassium. We suggest the following:
-In any 1000 mL-sized container of appropriate non-dextrose fluid, we suggest a maximum of 60 mEq of potassium.
-In a small-volume mini-bag of 100 to 200 mL of water that is to be infused into a peripheral vein, we suggest 10 mEq of potassium.
-In a small-volume mini-bag of 100 mL of water that is to be infused into a large central vein, we suggest a maximum of 40 mEq of potassium.
Intravenous potassium is most often infused in a peripheral vein at concentrations of 20 to 60 mEq/L in a non-dextrose-containing saline solution. Use of an infusion pump is preferred to prevent overly rapid potassium administration in any intravenous container with more than 40 mEq of potassium or if the desired rate of potassium administration is more than 10 mEq/hour.
Pain and phlebitis can occur during parenteral infusion of potassium into a peripheral vein. This primarily occurs at rates above 10 mEq/hour, but can be seen at lower rates. If pain occurs, either the infusion rate or, preferably, the potassium concentration should be reduced.
Once the hypokalemia is no longer severe, the rate of intravenous potassium repletion should be reduced or changed to oral therapy. Patients should be treated until the serum potassium concentration is persistently above 3.0 to 3.5 mEq/L and symptoms or signs attributable to hypokalemia have resolved.
3 notes
·
View notes
Note
hey! so i hope this isn’t too creepy/nosey, but im a medical student and i was reading your possible fibromyalgia post and have a couple ideas lol. full important disclaimer that im only partly into my studies and im currently in the hypochondriac phase and also your summary was amazing but a real doc would ask way more questions, so please consult with an actual doc and take everything i say with a grain of salt! but like your symptoms aren’t nothing so i would def encourage finding a doc that you trust to do a proper exam and run some tests. also im operating under the assumption that you’re under 50 lol, bc if you’re over 50ish that’s a whole diff list of possible diagnoses.
so the thirst thing you’re talking about is often called polydipsia and is commonly associated with diabetes insipidus. that’s not the normal diabetes you think about, but happens when your body can’t regulate fluids in your body properly. id think of this if you’re also peeing a lot lol. your doc would have to do some kidney tests for that, which wouldn’t be part of the blood panel you mentioned. i’m a little skeptical that it’s hypokalemia bc that would’ve showed up on your blood test results. it could be transient electrolyte imbalances when you exercise so have one of those electrolyte packets when you exercise lol, bc it never hurts to try the easy solutions first, but chronic low potassium should’ve shown up? tho eating sweet potatoes has never hurt.
other things it could be is a lower motor neuron problem bc you mentioned twitches and muscle weakness which is typical for those. i def can’t say more without tests, but look into/get your doc to look into myasthenia gravis or LEMS and see if either of those fit. i think it’s possible bc these often also start with face/upper body symptoms, but would need way more questions/tests to know. it’s unlikely but could also be a glycogen storage disease called McArdle disease bc you describe a second wind thing when you exercise along with exercise intolerance. that’s super rare tho so it’s unlikely unless someone in your family has it/has similar symptoms.
also look into autoimmune stuff like rheumatoid arthritis, lupus, and sjögrens disease. i have way less useful info on that bc we haven’t gotten to it in class yet lol, but sjögrens looks promising bc you often get dry mouth with it, and it often goes along with rheumatoid arthritis which could explain the joint stuff possibly.
it’s also totally possible this is fibromyalgia, but i would be cautious diagnosing it bc it often comes with fatigue and cognitive stuff which you didn’t mention. it’s also more of a pain thing, and doesn’t include your twitches/dry mouth. it’s def possible, and it was def something i thought of when i saw your symptoms, but personally i would want to rule out other stuff first bc fibromyalgia is pretty vague and often a diagnosis of exclusion when other things don’t fit.
sorry for overwhelming you!! i just saw your post and was like hmmm those symptoms sound like Something. again take my advice with a big grain of salt, but i do really think it’s worth asking your doc about it and getting tests done, bc even if there aren’t cures there are def treatments to help with a bunch of this stuff. it doesn’t sound urgent, but at least from your post your symptoms don’t sound like run of the mill aches and pains. hope you figure stuff out!!
The problem with 'muscles don't work right ouchy and I am also tired' is that it's a symptom for Absolutely Everything That Can Be Wrong With The Body. Is it cancer? Is it a terrible diet and sleep schedule? Who knows!
The doctor ran a diabetes test with the blood panel and it came up negative, but I don't know if that checks for weird kinds of diabetes. (Diabetes does not run in my family until we get very old.) That test was memorable because I have stupid fragile veins that freak out and collapse at the mere sight of a needle so I had to get stabbed nine times, they didn't manage to get the middle reading at all, and in the end they resorted to just stabbing my thumb with one of those diabetes home blood test thingies and manually squeezing my blood out into a tube drop by drop.
I looked up polydipsia and I don't think I have that. I think I just prefer my mouth to be wetter than my salival glands want it to be. 🤷♀️I think most of my problems are probably not related to any rare chronic disease, but just run-of-the-mill autism making it hard to look after myself or properly notice and process my physical condition and adapt accordingly. I don't eat enough fresh foods because it's hard to plan with the very short timeframe to prepare and eat them in. I'm uncoordinated and damage my body a lot through overwork or using muscles incorrectly because autism makes it hard to keep track of those things. My mouth feels dry and my skin feels itchy and my muscles feel sore because that's what being autistic feels like. My sleep schedule is garbage because my executive function is garbage and even once I do manage to get myself into the bed I can't just "go to sleep", I pass out when I'm ready to pass out.
I'm not saying it's impossible for anything else to be going on, but I think the known factor is the simplest explanation here. It's 2:30pm and I've been putting off breakfast for five hours. Every time I go into the kitchen I get distracted by housework instead. I am very hungry. This is not behaviour that is conducive to a well-functioning body.
126 notes
·
View notes
Text

EMERGENCY - Fatimah Suleman is a 28-year-old female studying in the Philippines away from her family in Somalia. One evening she called us and told us that she had constantly been having sharp stomach pain; we advised her to go to the hospital. She was then admitted to Baguio General Hospital and Medical Center with acute gastroenteritis with moderate signs of dehydration, hypokalemia, and major depressive disorder with psychotic symptoms.
Since being admitted, her condition has rapidly deteriorated. Here's what we know so far:
She suffered a major seizure that left her in a coma.
She was intubated, and a feeding tube was placed for two months.
When she awoke, her brain scans showed significant damage leaving her paralyzed. She now can't eat, breathe, speak, or go to the bathroom on her own.
Neurologically her brain function is not the same due to the severity of the seizure. Her whole body is clenched and tight. She is unable to move her limbs freely.
She then developed Hospital-Acquired Pneumonia from needing a constant trache/breathing tube.
She also developed a neurological disorder that pulls water from her brain cells as well as upper gastrointestinal bleeding.
Fatimah has a substantially difficult journey ahead of her. She is currently staying in a hospital and awaiting transport. We need help paying all her medical expenses in the Philippines and transporting her back to Somalia to recover with her family. Please keep Fatimah in your thoughts and prayers. Anything helps Fatimah's journey to recovery and reuniting her with her family. Thank you so much for taking the time to read Fatimah's story. God bless you.
161 notes
·
View notes
Text
woke up with a lot of muscle weakness, time to play the "is fludrocortisone giving me hypokalemia?" game
#I'm just gonna keep an eye on it for now but if it gets worse then it's ER time :/#cannot get a fucking break
14 notes
·
View notes
Photo

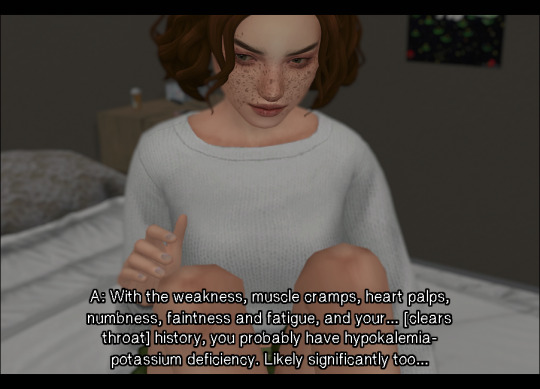


beginning | previous | next
november 4th, 7:47 pm
transcript:
Arya: You needed m-?
Dorothy: - I need you to be a nurse right now. And not someone who’s in love with my sister, okay?
A: Okay…
A: With the weakness, muscle cramps, heart palps, numbness, faintness and fatigue, and your… [clears throat] history, you probably have hypokalemia- potassium deficiency. Likely significantly too…
D: So, what? I just have to eat a banana or something?
A: Yeaaah, I wish it were that simple. You have a mild fever, you probably have an infection. Possibly an issue with your kidneys?
D: Okay.
A: You probably should go to the hospit-
D: -Yeah no, absolutely not.
A: [talking over Dee] OR Atleast an urgent care.
A: You think you’re gonna tell Bobbie?
Bobbie: [opening and closing door] Tell me what?
#virtuouscycle*#vcseriesfive#ts4#the sims 4#sims 4#ts4 story#sims 4 story#the sims 4 story#s4#simblr#ts4 simblr#simblr story#ts4 storytelling#simmer#ts4 simmer#sims 4 storytelling#illness tw#arya doing their best
30 notes
·
View notes
Note
how fast does Anders move around the house, given his low BCS and health problems? love that boy very much
Here’s an older video of Shuffles himself! Honestly, considering his body score and general health he gets around really well. His weird shuffle is due to his general muscle weakness and also hypokalemia. I’ve tried supplementing potassium but Anders is an AWFUL patient. It’s something Doc and I decided to not worry too much about because in the grand scheme of things it’s not going to change the outcome of his life. If he becomes so weak he’s unable to get around it’ll obviously be time to euthanize
#obviously if he was a normal cat we’d be more concerned with getting potassium into him regularly#but ultimately we decided the stress it causes him isn’t worth it#ask#Anders
261 notes
·
View notes